By | Medically Reviewed by Christopher W. Boelter, MD
|
Testosterone has always been recognized as the defining hormone of male physiology, but by 2025 medical science has moved far beyond the simplistic view that it only fuels sexual drive and muscle growth. Researchers now understand testosterone as a central regulator of men’s physical, emotional, and even cognitive well-being. Optimal levels support fertility, cardiovascular health, mood balance, and long-term vitality. When testosterone production falls, the consequences often extend across every area of life, from relationships to work performance.
This is why early recognition and accurate treatment of testosterone deficiency have become priorities in modern men’s health.
This article is written from the clinical perspective of John K. Matsuura MD, – Urologist in Advanced Precision Urology Medical Network (APUMN).
Role of Testosterone in Male Health
The role of testosterone is much broader than many men realize. Produced mainly in the testes under the control of the hypothalamic–pituitary–gonadal axis, it affects nearly every organ system. Adequate testosterone levels maintain lean muscle mass and prevent sarcopenia, preserve bone mineral density, and regulate fat distribution so that excess weight does not accumulate around the abdomen. On a mental health level, testosterone influences neurotransmitters associated with mood and motivation; low levels are strongly associated with fatigue, irritability, and in some cases major depressive symptoms.
Sexual function is another domain where testosterone is indispensable. While erections depend primarily on vascular and neurological factors, libido and sexual satisfaction are tightly linked to hormonal balance. Men with optimal testosterone typically report higher sexual confidence, spontaneous desire, and improved response to treatments for erectile dysfunction. By contrast, deficiency often leads to reduced interest in intimacy, lower frequency of morning erections, and difficulty maintaining sexual performance.
Symptoms of Low Testosterone
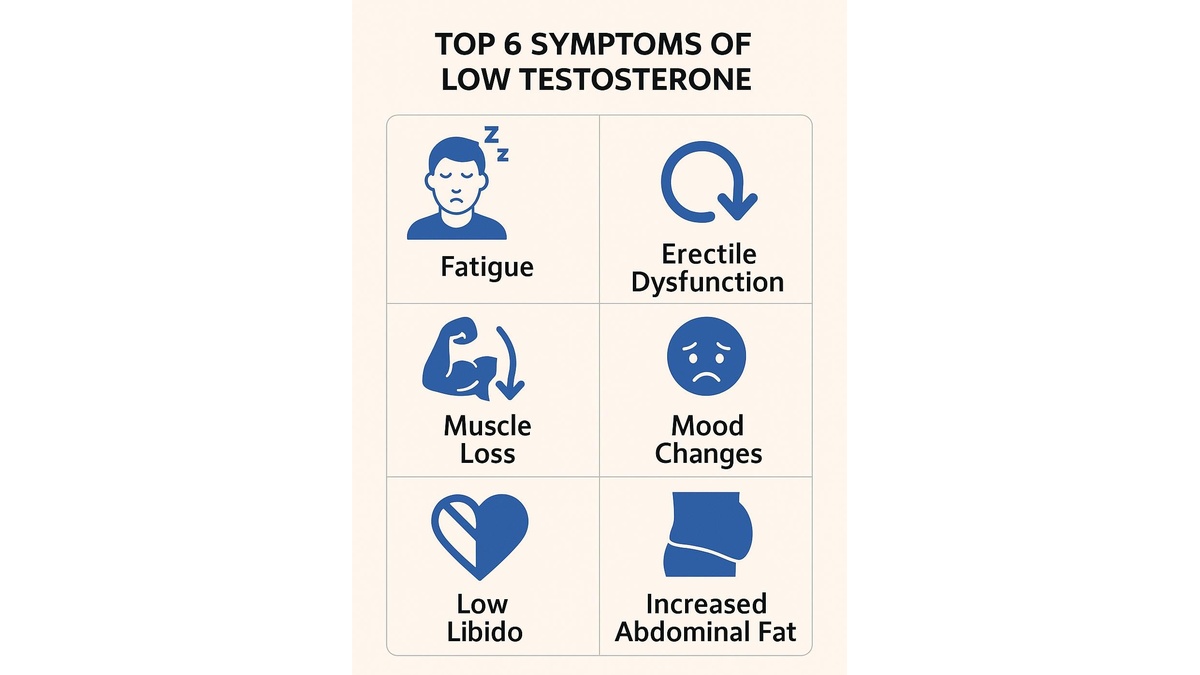
The challenge for both patients and doctors is that low testosterone does not manifest with a single unmistakable symptom. Instead, it produces a constellation of changes that can be subtle at first but grow more pronounced over time. Fatigue that does not improve with rest, loss of muscle tone despite regular exercise, mood instability ranging from irritability to depression, and diminished libido are among the most common complaints. Some men also notice increased abdominal fat and reduced body hair, while others experience erectile difficulties that do not respond fully to PDE5 inhibitors.
Top 6 Symptoms of Low Testosterone
What makes this even more complex is the overlap with other conditions. For example, depression alone can mimic fatigue and low libido, while obesity can independently reduce testosterone production. This is why self-diagnosis is unreliable, and professional evaluation is always required.
Many men first seek medical help because of sexual problems. Research in recent years has demonstrated that low testosterone and erectile dysfunction are closely connected. Sometimes testosterone therapy alone restores erectile performance, while in other cases combination therapy with PDE5 inhibitors is required. For a detailed look at how these treatments work together, see Viagra and Hormone Therapy: The Role of Testosterone When One Pill Isn’t Enough.
How Doctors Diagnose Testosterone Deficiency in 2025
By 2025, the diagnostic standards for testosterone deficiency have become more refined and patient-centered. The process begins with a thorough review of symptoms, since lab values alone are never enough to justify therapy. Doctors now emphasize the combination of clinical presentation and biochemical confirmation.
Blood testing remains the cornerstone. Because testosterone fluctuates during the day, guidelines recommend drawing blood in the early morning, ideally before 10 a.m., on two separate occasions. A total testosterone level below 300 ng/dL, especially when accompanied by consistent symptoms, is generally considered diagnostic of hypogonadism. For men whose results fall into the borderline range – between 300 and 400 ng/dL—measuring free testosterone provides more accuracy, as this fraction represents the biologically active hormone.
Further testing is often needed to identify the cause. Measuring luteinizing hormone (LH) and follicle-stimulating hormone (FSH) can distinguish between primary hypogonadism, where the testes fail to produce testosterone, and secondary hypogonadism, where the problem lies in the pituitary or hypothalamus. Prolactin testing may be performed when pituitary disease is suspected, and thyroid function tests are sometimes ordered because thyroid disorders can mimic symptoms of testosterone deficiency.
What sets 2025 apart is the integration of digital health tools. Many clinics now use artificial intelligence–driven risk calculators that combine lab data, patient age, body mass index, and reported symptoms. These models predict the likelihood of response to testosterone therapy and help doctors decide whether TRT is appropriate. Such personalized approaches minimize overtreatment while ensuring that men who genuinely need therapy receive it promptly.
The diagnostic process also includes ruling out reversible causes. Sleep apnea, obesity, excessive alcohol use, and certain medications are all known to suppress testosterone production. Addressing these factors before or alongside therapy can sometimes restore natural hormone balance without the need for long-term replacement.
Testosterone Replacement Therapy (TRT): Forms Available in 2025
In 2025, testosterone replacement therapy has become both safer and more individualized than in previous decades. Instead of a one-size-fits-all approach, men can choose among multiple delivery systems, each with unique advantages and limitations. The most widely used options are topical gels, intramuscular injections, skin patches, and subcutaneous pellets.
Topical gels
Topical gels remain the most popular option because they provide steady hormone levels and are easy to apply daily. However, they carry a risk of transferring testosterone to others through skin contact, which is why doctors emphasize careful application and handwashing.
Injections
Injections, typically administered every one to two weeks, deliver reliable results but may cause fluctuations in mood and energy when levels peak and then decline. Some clinics now use longer-acting injectable formulations that last up to three months, improving stability and convenience.
Patches
Patches are applied to the skin daily and provide steady absorption. Skin irritation remains their main drawback, but newer adhesive technologies have improved tolerability.
Pellets
Pellets, small cylinders implanted under the skin every three to six months, release testosterone gradually. They are convenient for men who prefer not to manage daily or weekly dosing, though the minor surgical procedure and cost are considerations.
Risks and Contraindications of TRT
While testosterone therapy can significantly improve quality of life for men with hypogonadism, it is not risk-free. The most important principle in 2025 remains: therapy should only be prescribed to men with documented low testosterone and symptoms.
Potential risks include increased red blood cell count (polycythemia), which raises the chance of blood clots if not monitored. Prostate health is another concern. Current evidence shows that TRT does not cause prostate cancer, but it can accelerate growth in men who already have prostate disease, so regular PSA testing and digital rectal exams are recommended. Sleep apnea may worsen with testosterone therapy, and men with untreated severe heart failure or recent cardiovascular events are advised against it.
Contraindications include diagnosed prostate or breast cancer, hematocrit above 54%, uncontrolled sleep apnea, and recent myocardial infarction or stroke. In such cases, lifestyle and non-hormonal strategies should be prioritized.
Doctors today carefully balance these risks against the benefits. For men who suffer from persistent fatigue, muscle weakness, depression, and erectile dysfunction due to low testosterone, TRT can be life-changing. But safety requires ongoing monitoring, including regular blood counts, PSA levels, and hormone checks.
Table: Comparison of TRT Forms in 2025
| Form | Pros | Cons | Cost (approx, US) |
| Gel (topical) | Easy daily use, steady levels | Risk of transfer to others, daily commitment | $30–$150/month |
| Injections (IM/SC) | High efficacy, lower cost, long-acting versions available | Peaks and troughs, requires needles/clinic visits | $20–$100/month |
| Patch | Convenient, steady absorption | Skin irritation, visible on skin | $50–$200/month |
| Pellets (implants) | Long duration (3–6 months), no daily dosing | Minor surgery, higher upfront cost | $400–$1,000/procedure |
TRT and Erectile Dysfunction After Prostate Cancer
One of the most debated topics is whether men who have undergone prostate cancer treatment can safely use testosterone therapy. Until recently, TRT was considered absolutely contraindicated in this group. However, modern research suggests that carefully selected men – those with low-risk cancer treated successfully and with stable PSA — may benefit from therapy under strict medical supervision.
Erectile dysfunction after prostate cancer surgery or radiation often has a neurovascular component, meaning nerve and blood vessel damage. In such cases, testosterone therapy alone may not restore function, but when combined with PDE5 inhibitors or penile rehabilitation programs, it can improve outcomes. For a detailed discussion of this delicate topic, see Erectile Dysfunction After Prostate Cancer Treatment: A Neurovascular Urologic Approach.
Lifestyle and Natural Strategies to Boost Testosterone
Not every man with low testosterone requires hormone replacement. In 2025, clinicians emphasize that lifestyle interventions remain the first line of defense, particularly for men with borderline levels or those who cannot safely undergo TRT.
Regular physical activity is one of the strongest natural boosters of testosterone. Resistance training, especially compound movements like squats and deadlifts, stimulates testosterone release and prevents age-related muscle loss. High-intensity interval training (HIIT) has also been shown to improve both hormonal balance and cardiovascular health.
Nutrition plays an equally important role. Diets rich in lean protein, healthy fats, and micronutrients such as zinc and vitamin D support testosterone production. On the other hand, excessive processed foods, sugar, and alcohol are linked to obesity and metabolic syndrome, both of which suppress natural testosterone.
Sleep quality is another overlooked factor. Men who consistently get fewer than six hours of sleep per night often present with significantly lower testosterone levels. Restorative sleep regulates cortisol, a stress hormone that competes with testosterone and contributes to abdominal fat gain. Stress management itself is a critical component: mindfulness, yoga, and relaxation techniques not only reduce cortisol but also improve mental health, which indirectly supports healthy testosterone.
These non-pharmacological strategies can, in some cases, restore testosterone to a functional range without medication. Even when men start TRT, maintaining good lifestyle habits maximizes therapy effectiveness and reduces risks.
Testosterone Therapy Combined with Erectile Dysfunction Treatment
For many men, low testosterone and erectile dysfunction coexist. In fact, it is estimated that up to 30–40% of men with hypogonadism report erectile difficulties. In these cases, TRT alone may not fully restore erectile function. The combination of testosterone therapy and PDE5 inhibitors such as sildenafil or tadalafil often delivers superior outcomes.
TRT improves libido, mood, and energy, while PDE5 inhibitors enhance the physiological mechanisms of erections by increasing penile blood flow. When used together, men who previously did not respond well to PDE5 inhibitors alone often regain satisfactory sexual performance.
This combined approach is particularly important for men recovering from chronic illnesses or prostate-related procedures, where both vascular and hormonal factors contribute to dysfunction. For a practical guide on regaining sexual health through combined therapy and confidence-building strategies, see Erectile Dysfunction: How to Regain Strength and Confidence.
Frequently Asked Questions (FAQ)
What are the earliest signs of low testosterone in men?
Men often notice fatigue, reduced sexual desire, and mood changes before more obvious symptoms like muscle loss appear. These early signs should prompt a doctor’s evaluation and blood testing.
Can lifestyle changes alone raise testosterone?
Yes, in many men with borderline low levels, weight loss, regular exercise, better sleep, and stress management significantly improve testosterone production. Lifestyle is always the foundation of treatment.
Is testosterone replacement therapy safe long-term?
When monitored correctly, TRT is generally safe. Doctors track blood counts, PSA levels, and cardiovascular health to minimize risks over time.
Do all men with erectile dysfunction need testosterone therapy?
No, erectile dysfunction has many causes, and not all are hormonal. Only men with confirmed low testosterone and symptoms should consider TRT, often combined with PDE5 inhibitors for best results.
Can testosterone therapy be used after prostate cancer?
In carefully selected men with successfully treated, low-risk cancer and stable PSA, TRT may be considered under strict medical supervision. Decisions are always individualized.
Does age alone mean I need TRT?
Not necessarily. Testosterone levels naturally decline with age, but therapy is only recommended when symptoms and lab results both indicate clinically significant deficiency.
References
- Mayo Clinic: Testosterone therapy, potential benefits and risks
- Cleveland Clinic: Low testosterone (male hypogonadism), symptoms and treatment
- Endocrine Society: Clinical practice guidelines on testosterone therapy
- PubMed: TRAVERSE trial (NEJM 2023) on cardiovascular safety of testosterone replacement therapy
- American Urological Association: Testosterone deficiency guideline
- Zitzmann et al. (2025): CV safety of testosterone therapy post-TRAVERSE position statement
- Cruickshank et al.: meta-analysis on effects and safety of testosterone replacement therapy
