What is Peyronie’s Disease?
Peyronie’s disease is a connective tissue disorder of the penis, defined by the formation of fibrous scar tissue (plaques) within the tunica albuginea, the fibrous sheath that surrounds the erectile bodies (corpora cavernosa). This tissue, normally elastic, becomes rigid and prevents symmetrical expansion of the penis during erection. The result is penile curvature, deformity, shortening, and sometimes pain or erectile dysfunction (ED).
The disease was first described in 1743 by French surgeon François de la Peyronie. For centuries, it was considered rare, but research over the past 20 years has revealed that it is far more common than previously thought. Modern studies suggest prevalence rates of up to 10–13% of adult men, though actual numbers may be higher since many men never seek medical help due to embarrassment or misconceptions.
It is important to note that Peyronie’s disease is benign. It is not cancer, and it is not contagious. However, its impact can be significant, affecting sexual confidence, psychological well-being, and intimate relationships.
How Peyronie’s Disease Develops: Pathophysiology
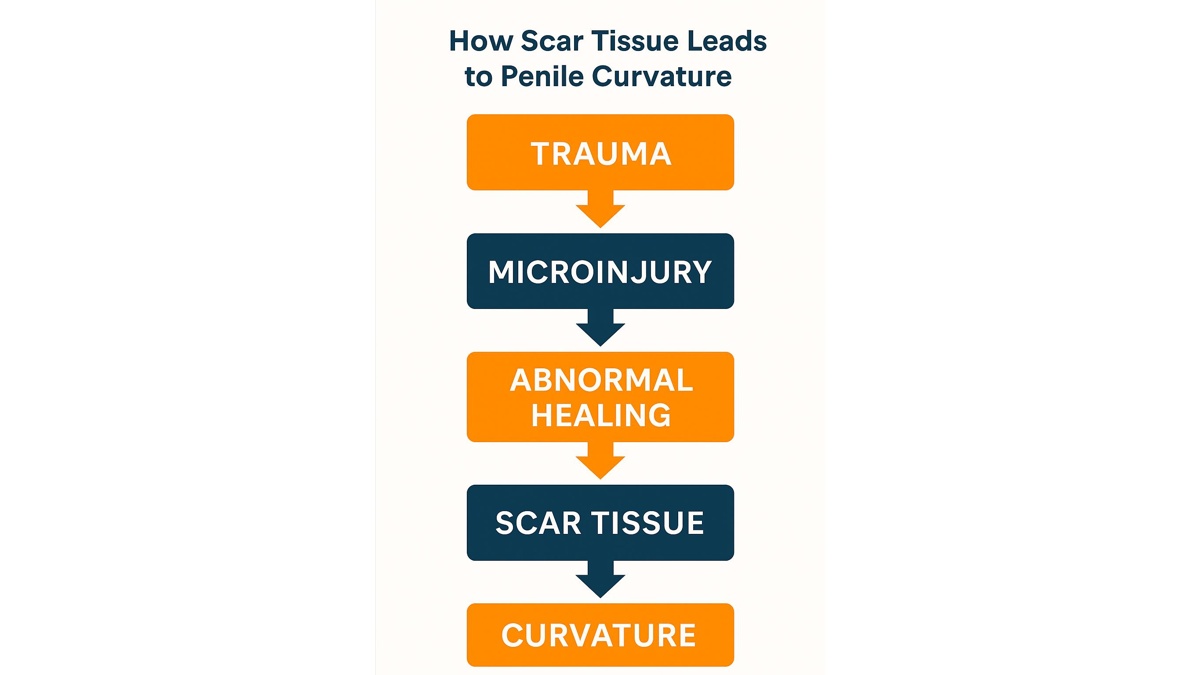
- Microtrauma to the penis — often during sexual intercourse, sports, or even spontaneous erections — causes small tears in the tunica albuginea.
- Instead of normal wound healing, there is abnormal fibroblast activity. Collagen and fibrin are deposited excessively.
- Chronic inflammation persists, with involvement of cytokines such as transforming growth factor-beta (TGF-β).
- A fibrous plaque forms. Over time, this hardened scar tissue loses elasticity, preventing even expansion during erection.
- The result is bending or curvature toward the side of the plaque. Some men also develop hourglass narrowing or penile shortening.
Recent genetic and molecular studies (PubMed, 2024) suggest that certain men have a genetic predisposition to abnormal wound healing and fibrosis, which explains why not all men with penile trauma develop Peyronie’s disease.
Causes and Risk Factors of Peyronie’s Disease
Penile Trauma and Micro-Injury
The most widely accepted trigger is repetitive microtrauma, especially during vigorous or unconventional sexual activity. Unlike major penile fractures, these micro-injuries often go unnoticed but initiate an abnormal healing process.
Genetic Predisposition
A strong association has been documented between Peyronie’s disease and Dupuytren’s contracture (a fibrotic condition of the hand). Both share genetic markers linked to collagen metabolism. Men with family history of fibrotic disorders may have a higher susceptibility.
Age and Connective Tissue Changes
The risk increases significantly after age 40. With aging, the tunica albuginea loses elasticity, and tissue repair slows. Most men diagnosed with Peyronie’s fall between 40 and 70 years old.
Vascular and Metabolic Health
- Diabetes mellitus (linked with both ED and abnormal wound repair).
- Hypertension and atherosclerosis (reduce penile blood flow).
- Smoking (damages microcirculation).
Hormonal Factors
Some studies indicate that low testosterone may worsen fibrotic activity, though the evidence remains under investigation in 2025.
Epidemiology and Global Trends
- USA and Europe: 8–13% of men, with higher detection thanks to awareness campaigns.
- Asia: Lower reported prevalence (~3–5%), but experts believe underreporting is common due to cultural stigma.
- Trends (2020–2025): More diagnoses in younger men (30s–40s), likely due to increased awareness and widespread use of erectile health clinics.
Psychological and Sexual Impact
- Sexual dysfunction: Men often report painful erections, difficulty with penetration, or complete inability to have intercourse.
- Body image issues: Penile deformity can cause embarrassment and avoidance of intimacy.
- Mental health: Rates of depression and anxiety are significantly higher among men with Peyronie’s disease (PubMed, 2023 review).
- Relationships: Communication difficulties, reduced sexual satisfaction, and strain on partnerships are common.
In surveys, over 50% of affected men describe Peyronie’s as having a “severe or very severe” impact on quality of life, even if the curvature is moderate.
Symptoms and Stages of Peyronie’s Disease
Peyronie’s disease is not a static condition. It typically progresses through two distinct phases, which play a central role in determining the right treatment strategy.
The acute (or active) phase usually lasts from six to eighteen months. During this period, men often notice pain during erections, the gradual appearance of penile curvature, and the development of a palpable plaque beneath the skin. The deformity may worsen as the scar tissue matures, and the uncertainty of change often causes significant anxiety.
After one to two years, the condition usually enters the chronic (or stable) phase. At this stage, pain tends to diminish or disappear, but the curvature remains fixed. Men may also notice penile shortening, indentation (sometimes described as an “hourglass” deformity), or narrowing of the shaft. Erectile dysfunction becomes more common once the disease stabilizes, not only because of tissue rigidity but also due to the psychological burden it carries.
Conservative Treatments for Peyronie’s Disease
Conservative treatment options aim to relieve symptoms and improve penile function, particularly during the acute stage. While they may not completely reverse curvature, they can help reduce pain, soften plaques, and prevent progression.
Oral therapies have historically been the first line of management. Agents such as pentoxifylline, which enhances microcirculation, and coenzyme Q10 have shown some benefit. Vitamin E and Potaba have been used for decades, though evidence supporting their effectiveness remains weak. Current guidelines from the American Urological Association (AUA) and European Association of Urology (EAU) emphasize that oral medications alone have limited value, but they may still contribute as part of a multimodal regimen.
In contrast, injection therapies have demonstrated stronger outcomes. Collagenase clostridium histolyticum (Xiaflex) is the only FDA-approved drug for Peyronie’s disease and is widely used in North America and Europe. It works by breaking down excess collagen within plaques and, in clinical studies, has reduced curvature by roughly 30–35% on average. When collagenase is not available, agents like verapamil or interferon-alpha-2b may be injected directly into plaques. These drugs are less effective but can decrease pain and soften hardened tissue.
Mechanical approaches are also central to non-surgical treatment. Penile traction therapy (PTT) involves applying gentle, sustained stretching using a medical device. When performed regularly, it can improve curvature and help preserve length. Vacuum erection devices (VEDs), which create negative pressure to draw blood into the penis, have also been used to maintain elasticity and prevent shortening. Increasingly, urologists recommend combining mechanical methods with medication for optimal outcomes.
The most promising results are seen with combination therapy. For example, collagenase injections followed by traction therapy maximize curvature reduction. Similarly, pentoxifylline paired with traction or VED use may offer synergistic benefits. For men who also suffer from erectile dysfunction, phosphodiesterase type 5 inhibitors (such as sildenafil or tadalafil) are frequently prescribed. These drugs do not treat Peyronie’s plaques directly but help restore sexual function, which is critical for quality of life.
Treatment Options for Peyronie’s Disease
| Treatment Type | Example/Method | Pros | Cons | Best For |
|---|---|---|---|---|
| Oral Medications | Pentoxifylline, Vitamin E, CoQ10 | Widely available, inexpensive, may reduce pain | Limited proven effect on curvature | Early or mild disease |
| Injections | Collagenase (Xiaflex), Verapamil, Interferon | Strongest evidence for curvature improvement | Pain, bruising, cost; collagenase not available everywhere | Moderate curvature in active phase |
| Traction Devices | Penile traction therapy (PTT) | Preserves length, non-invasive, can improve curvature | Requires daily use and patience | Men motivated for conservative therapy |
| Vacuum Devices | Vacuum erection devices (VEDs) | Improve blood flow, maintain elasticity, safe | Less impact on curvature alone | Adjunct therapy, penile rehabilitation |
| Combination | Collagenase + traction; oral meds + PTT/VED | Synergistic effect, better outcomes | Requires compliance and monitoring | Most men in the active phase |
Surgical Treatment Options for Peyronie’s Disease
When conservative measures are insufficient, surgery remains the gold standard. By 2025, surgical techniques have become safer and more refined, with outcomes depending on curvature severity, erectile function, and patient preference.
Tunical Plication (Nesbit or Modified Plication)
This is the most common and straightforward approach. Sutures are placed on the side opposite the plaque, shortening that side so the penis straightens. Plication has a high success rate (80–90% of men achieve functional straightening). The main drawback is some penile shortening, which can be concerning for men who already notice loss of length.
Plaque Incision/Excision with Grafting
For more severe curvatures (typically >60 degrees) or complex deformities such as hourglass narrowing, surgeons may cut into or remove part of the plaque and insert a graft to restore symmetry. This preserves length but carries higher risks, including erectile dysfunction and altered sensation. Advances in graft materials such as porcine small intestinal submucosa and synthetic biologics have improved durability compared with older options.
Penile Prosthesis Implantation
In men with Peyronie’s disease combined with severe erectile dysfunction unresponsive to medications, a penile prosthesis offers both straightening and rigidity. Inflatable devices are most commonly used in 2025. Modern surgical protocols allow simultaneous modeling of curvature during prosthesis placement, often eliminating the need for additional grafting.
Peyronie’s Disease and Erectile Dysfunction
The relationship between Peyronie’s disease and erectile dysfunction is strong and bidirectional. Scar tissue not only causes physical curvature but also disrupts normal hemodynamics within the penis. Men often find that erections are weaker or incomplete, particularly if plaques interfere with venous occlusion.
Psychological factors intensify the problem. Anxiety, depression, and loss of sexual confidence are highly prevalent. Studies published on PubMed (2023–2024) show that men with Peyronie’s disease are more than twice as likely to report erectile dysfunction compared with peers without the condition.
Treatment is tailored:
- In men with intact erections but bothersome curvature, traction, injections, or surgery may be sufficient.
- For those with both Peyronie’s and erectile dysfunction, PDE5 inhibitors (Viagra, Cialis) are often prescribed first.
- In post-prostate cancer patients, Peyronie’s may complicate rehabilitation further; combined approaches are required.
See more on this: Erectile Dysfunction After Prostate Cancer Treatment: A Neurovascular Urologic Approach
FAQ: Peyronie’s Disease in 2025
Is Peyronie’s disease common?
Yes. Recent studies suggest that up to 13% of men may be affected, though many remain undiagnosed due to stigma.
Can Peyronie’s disease go away on its own?
Spontaneous resolution is rare. In most cases, the curvature stabilizes after the acute phase but does not completely disappear without treatment.
What is the newest non-surgical therapy?
Collagenase clostridium histolyticum (Xiaflex) remains the leading injectable therapy in 2025, often combined with traction devices for maximum effect.
Does surgery cure Peyronie’s?
Surgery offers the most definitive correction, particularly for severe curvature. However, it does not prevent new plaques from forming, and risks such as shortening or erectile dysfunction remain.
Can Peyronie’s disease cause erectile dysfunction?
Yes, both mechanical and psychological mechanisms contribute. Scar tissue alters erection quality, and emotional stress worsens the impact.
Are supplements effective for Peyronie’s disease?
Evidence is limited. Some men use vitamin E, CoQ10, or pentoxifylline, but these are best seen as adjuncts rather than stand-alone therapies.
How does Peyronie’s disease affect relationships?
Many couples experience strain due to reduced sexual satisfaction. Open communication and, when needed, counseling or sex therapy can help manage the emotional burden.
