Testosterone therapy, particularly in its injectable form, has become one of the most discussed interventions in modern men’s health. Over the past decade, prescriptions have increased in the United States, partly fueled by promises of renewed vitality and energy. Yet, according to current American Urological Association (AUA) and Endocrine Society guidelines, injectable testosterone therapy should be considered only when a true testosterone deficiency clinically known as hypogonadism is confirmed. This requires both the presence of characteristic symptoms and clear laboratory evidence of low testosterone levels. Treating a laboratory number without understanding its cause can expose patients to unnecessary risks and mask other underlying disorders.
The essence of appropriate testosterone replacement therapy (TRT) lies in diagnostic precision. Symptoms such as low libido, chronic fatigue, mood disturbances, and decreased muscle mass may suggest hormonal imbalance, but they are not specific to testosterone deficiency. Only when these clinical signs coexist with persistently low biochemical values does TRT become medically justified.
How to diagnose testosterone deficiency and confirm therapy necessity
Symptoms and Laboratory Criteria: Defining True Hypogonadism
The evaluation begins with careful documentation of symptoms that may interfere with a man’s quality of life. Many men with testosterone deficiency describe diminished sexual interest, reduced strength, and general lethargy. Others notice changes in mood, sleep, or mental focus. However, because these complaints overlap with common age-related and psychosocial conditions, objective confirmation through laboratory testing is indispensable.
Modern endocrine and urological practice recommends measuring total testosterone early in the morning, ideally between seven and ten a.m., when hormone levels are at their daily peak. Two separate tests, performed at least a week apart, are required to confirm consistently low levels. In most U.S. laboratories, a morning total testosterone concentration below 300 ng/dL (10.4 nmol/L) is considered low, though interpretation must always reflect the specific reference range used by the testing facility. When results fall into a borderline zone or when sex hormone-binding globulin (SHBG) is abnormally high or low, the measurement of free testosterone becomes necessary to provide a clearer picture of hormonal availability.
Certain factors such as illness, insufficient sleep, alcohol use, obesity, or medications like opioids and corticosteroids can transiently lower testosterone. For that reason, repeat testing under stable conditions is essential before making any treatment decision. The Endocrine Society’s 2024 update emphasizes that at least two consistent results are needed to diagnose hypogonadism reliably.
In clinical practice, this diagnostic rigor prevents overdiagnosis and ensures that testosterone therapy is reserved for men who can genuinely benefit from it. A single abnormal test should never serve as the basis for initiating lifelong hormone therapy.
Causes of Hypogonadism: Primary, Secondary, and Functional
Understanding the origin of testosterone deficiency determines not only whether replacement therapy is necessary but also which approach will yield the best outcome. Endocrinologists classify hypogonadism as primary or secondary depending on whether the dysfunction originates in the testes or the hypothalamic–pituitary axis.
In primary hypogonadism, the testes themselves fail to produce adequate testosterone despite normal or elevated levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This situation may occur in genetic conditions such as Klinefelter syndrome, after testicular trauma, or following chemotherapy and radiation. Aging can also contribute to a gradual decline in testicular output, though not every older man meets the clinical definition of hypogonadism.
Secondary hypogonadism, by contrast, arises when the pituitary gland or hypothalamus fails to stimulate the testes appropriately. Tumors of the pituitary, elevated prolactin levels, head trauma, or systemic illnesses can all disrupt this hormonal communication. The laboratory pattern in these cases typically shows both low testosterone and inappropriately low or normal LH and FSH levels.
A third, increasingly recognized form functional hypogonadism is driven by metabolic and lifestyle factors rather than structural disease. Obesity, type 2 diabetes, chronic stress, and sleep apnea can suppress normal gonadotropin release. The good news is that functional hypogonadism may be reversible with targeted lifestyle modifications, weight management, and treatment of the underlying condition.
Distinguishing between these types is critical. Primary hypogonadism usually requires direct testosterone replacement, whereas secondary or functional forms may improve once the precipitating factor is corrected. Accurate classification also informs fertility discussions, as external testosterone can suppress sperm production, making it unsuitable for men actively trying to conceive.
Choosing the Right Form of Therapy: Injections, Gels, or Pellets
Among available options for testosterone replacement, injections remain the most commonly prescribed in the United States. They offer predictable dosing, lower cost per milligram, and convenient administration intervals typically every one to two weeks for short-acting formulations or every ten to twelve weeks for long-acting esters. For men who value simplicity and prefer less frequent interventions, injectable testosterone can be a practical solution.
Nevertheless, injections are not ideal for everyone. The peaks and troughs that accompany intramuscular dosing can lead to fluctuations in mood, energy, and libido. Self-administration requires proper training, and periodic blood monitoring is necessary to track hematocrit, prostate-specific antigen (PSA), and lipid profiles.
For men who prefer more stable hormone levels, transdermal gels offer a daily, non-invasive alternative. These formulations allow precise dose adjustments but require caution to avoid skin-to-skin transfer to others. Subcutaneous pellets, implanted under the skin every few months, provide another long-acting choice, though they require a minor office procedure for insertion and removal. In 2025, intranasal formulations are also available in the U.S. market, offering a short-acting option suitable for men who prefer flexibility and lower systemic exposure.
Ultimately, no single route fits all patients. According to the AUA’s 2024 guideline revision, the best approach involves shared decision-making between patient and clinician, balancing convenience, cost, comorbidities, and personal preference. What matters most is ensuring that any form of testosterone therapy is based on a confirmed medical need rather than on the pursuit of non-specific well-being or age-related optimization.
Contraindications and Relative Risks of Testosterone Injection Therapy
Even though injectable testosterone remains one of the most effective approaches to treat clinically confirmed hypogonadism, it is not appropriate for every man. Both the American Urological Association and the Endocrine Society emphasize that testosterone therapy must follow a careful, evidence-based evaluation that includes screening for absolute and relative contraindications.
Therapy should be strictly avoided in men with prostate or breast cancer, untreated severe obstructive sleep apnea, hematocrit levels above 54%, recent myocardial infarction or stroke, or uncontrolled heart failure. These conditions significantly increase the risk of adverse outcomes when androgens are introduced.
Relative contraindications include conditions that do not automatically exclude treatment but demand close supervision for example, moderate benign prostatic hyperplasia, controlled cardiovascular disease, borderline hematocrit, or sleep apnea treated with CPAP.
The physiological risks of testosterone therapy stem from its systemic actions. Elevated red blood cell production may lead to erythrocytosis, increasing blood viscosity and thrombosis risk. Some men experience mild fluid retention or blood pressure elevation. Recent FDA labeling revisions in 2025 highlight the need for blood-pressure monitoring and emphasize the possible cardiovascular implications of long-term therapy.
Monitoring remains the cornerstone of safety. During the first year of treatment, men should be evaluated every three to six months, then annually once stable. Each visit includes assessment of hematocrit, prostate-specific antigen (PSA), lipid profile, liver enzymes, and cardiovascular parameters. Proper follow-up transforms testosterone therapy from a potentially risky intervention into a controlled, reversible medical procedure.
| Contraindication / Risk | Description | Monitoring / Mitigation |
|---|---|---|
| Prostate or breast cancer | Androgen-responsive tumor | PSA baseline and repeat testing, urologic follow-up |
| Hematocrit > 54% | Increased blood viscosity | Pause therapy, therapeutic phlebotomy if required |
| Severe OSA | Risk of worsening hypoxia | Manage with CPAP before therapy |
| Recent MI or stroke | Cardiovascular instability | Cardiologist clearance before start |
| Fertility desire | TRT suppresses spermatogenesis | Consider hCG or clomiphene instead |
These recommendations reflect a broader principle of modern endocrinology testosterone should restore normal physiology, not enhance it beyond natural limits. Replacement is a therapy, not an optimization tool.
Effects of testosterone injections on male fertility and how to minimize risks
Expected Effects and Realistic Timeframes
Understanding the timeline of expected benefits helps align medical goals with patient expectations. Injectable testosterone does not act overnight; hormonal balance builds gradually, and improvements emerge in distinct phases.
Within the first month, many men report an increase in libido and morning erections. Mood and energy typically follow several weeks later. Over the subsequent months, muscle strength and lean mass improve, while fat percentage declines modestly. Skeletal benefits, such as increased bone mineral density, take the longest sometimes up to two years because bone remodeling is a slow biological process.
A realistic perspective allows men to appreciate progress without unrealistic hopes of an immediate transformation. The therapy works best when combined with consistent exercise, balanced nutrition, and sufficient sleep, which potentiate its anabolic and metabolic effects.
Below is a concise graphical representation summarizing this timeline:
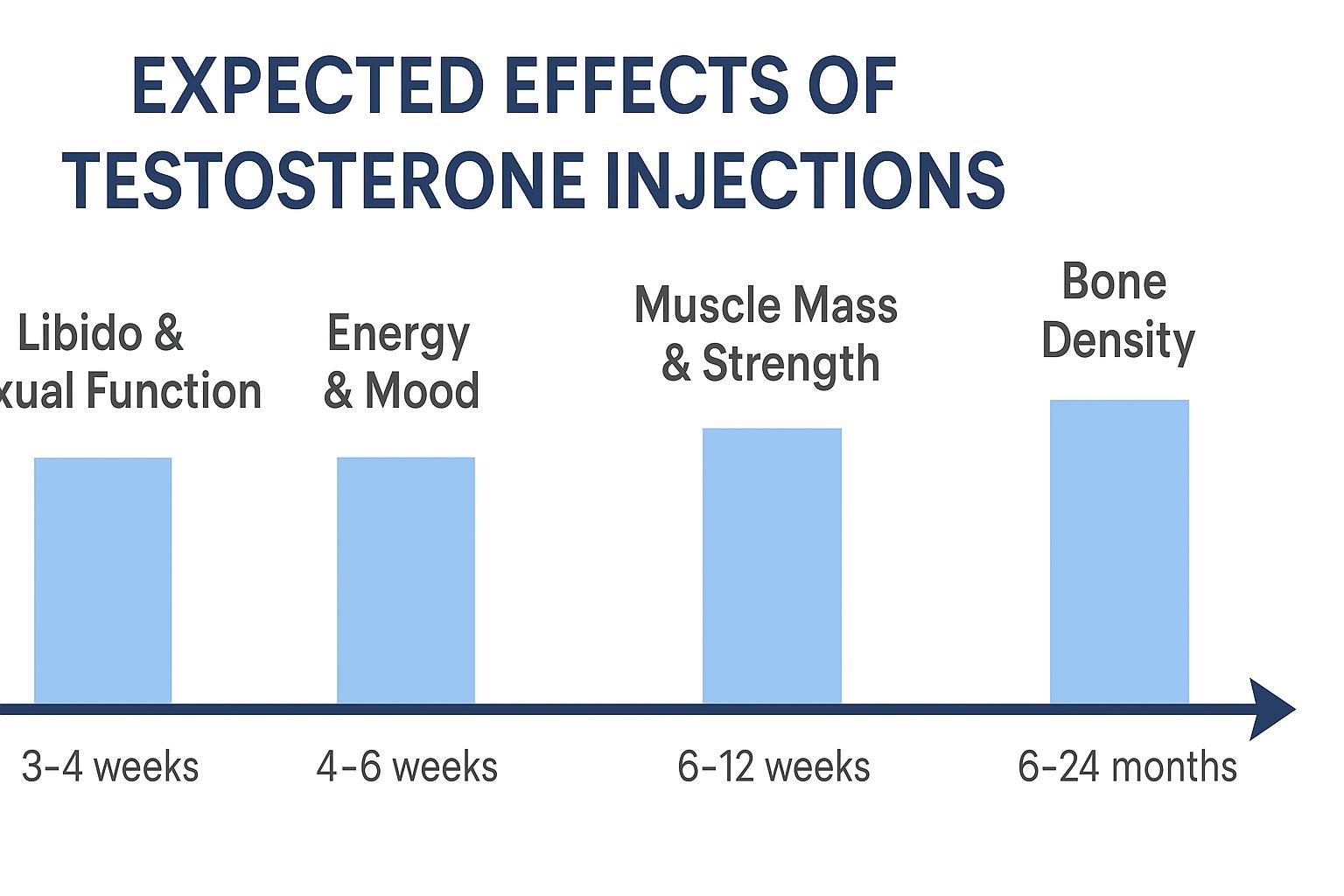
Gradual onset of testosterone benefits over time libido and sexual function improve within weeks, followed by gains in energy, muscle strength, and bone density across several months to two years (based on data from AUA 2024 and Mayo Clinic 2025).
Injectable testosterone is thus a gradual therapy, whose success depends on medical precision and patient persistence rather than the pursuit of immediate performance gains.
Diagnostic Flowchart: From Suspicion to Treatment Decision
The decision to begin injectable testosterone therapy must follow a structured and reproducible pathway. Physicians typically move from symptom recognition to biochemical confirmation, then to etiologic differentiation and exclusion of contraindications. Only after that can therapy safely begin.
The diagnostic sequence proceeds through the following stages: identifying clinical symptoms of androgen deficiency, measuring morning total and free testosterone twice on separate days, confirming persistent low levels, assessing LH, FSH, prolactin, and SHBG to determine whether the condition is primary or secondary, and ruling out reversible causes such as obesity, sleep apnea, or medication effects. Once contraindications are excluded, shared decision-making determines the best route of replacement injection, gel, or pellet.
This process is summarized in the clinical algorithm below.

This structured flow ensures that only men with confirmed, symptomatic testosterone deficiency and without major contraindications receive injectable testosterone therapy. It protects patients from unnecessary hormone use while ensuring timely treatment for those who truly need it.
Key Takeaway
Injectable testosterone therapy has clear, evidence-based indications. It should be prescribed only after biochemical confirmation of hypogonadism and exclusion of contraindications. The safest and most effective outcomes occur when therapy is guided by specialists, monitored closely, and combined with healthy lifestyle interventions. Testosterone replacement is a valuable medical treatment, not an anti-aging trend, and, when applied correctly, it restores physiological balance and quality of life to men who truly need it.
Frequently Asked Questions (FAQ)
When should men consider testosterone injections instead of other forms of therapy?
Injections are generally preferred when long-term adherence is a concern or when patients desire less frequent dosing. They are also appropriate for men who do not achieve adequate testosterone levels with gels or transdermal options. However, the decision must always follow confirmation of true hypogonadism through laboratory testing.
Can testosterone injections be used for age-related fatigue or low energy alone?
No. Current medical consensus from the American Urological Association and the Endocrine Society (2024–2025) clearly states that testosterone therapy is indicated only for men with documented testosterone deficiency and relevant symptoms. Using injections solely for “low energy” or aging-related decline is not supported by evidence and may expose patients to unnecessary risks.
How often do testosterone injections need to be given?
The frequency depends on the preparation. Short-acting formulations such as testosterone cypionate or enanthate are administered every one to two weeks. Long-acting undecanoate formulations may last up to ten or twelve weeks. Dosage schedules should always be individualized based on trough testosterone levels and clinical response.
What happens if testosterone therapy is stopped?
Once injections are discontinued, testosterone levels gradually return to baseline within several weeks. Symptoms of deficiency may reappear, particularly if the underlying cause of hypogonadism remains unresolved. The process is reversible, and discontinuation does not cause permanent hormonal damage when managed appropriately.
Does testosterone replacement increase prostate cancer risk?
Current data do not show a direct causal link between physiologic testosterone replacement and prostate cancer. However, men on therapy require periodic prostate monitoring through PSA testing and digital rectal examination, as testosterone can stimulate the growth of existing, undiagnosed malignancies.
Will testosterone injections affect fertility?
Yes. Exogenous testosterone suppresses the pituitary release of LH and FSH, which in turn decreases sperm production. Men wishing to preserve fertility should consider alternatives such as human chorionic gonadotropin (hCG) or selective estrogen receptor modulators like clomiphene citrate.
Are the cardiovascular risks of testosterone therapy real?
Recent FDA updates (February 2025) highlight that testosterone products can influence blood pressure and may interact with preexisting cardiovascular conditions. Nevertheless, large controlled studies show that when therapy is appropriately prescribed and monitored, the absolute cardiovascular risk remains low.
How long does it take to feel the benefits of testosterone injections?
Some improvements, such as libido and mood, appear within a few weeks, while changes in body composition and bone strength may take months to a year. Patience and regular monitoring are essential to achieve sustainable results.
References
- American Urological Association (AUA) – Testosterone Deficiency Guideline
- Endocrine Society – Guideline Resources on Testosterone Therapy for Hypogonadism
- U.S. Food and Drug Administration (FDA) – Class-wide Labeling Changes for Testosterone Products (Feb 28, 2025)
- Article: In Brief – Label Changes for Testosterone Products
- Review: Testosterone Deficiency and Treatments – Common Misconceptions
