Testosterone is the cornerstone hormone of male health, influencing everything from sexual function and muscle mass to mood, energy, and bone density. Over the past two decades, interest in testosterone levels among American men has grown rapidly. According to the Urology Times (2023), average testosterone concentrations in young men have been steadily declining in the U.S., likely due to obesity, sedentary lifestyle, poor sleep, and environmental factors.
Clinical cases when testosterone injections are truly indicated
This article provides a science-based 2025 guide to understanding testosterone: what it is, how it functions, normal levels, and when correction is truly needed. The content follows modern U.S. clinical guidelines (American Urological Association, Endocrine Society) and presents evidence-based approaches to maintaining hormonal balance safely.
Understanding Testosterone and Its Regulation
What is Testosterone?
Testosterone is a steroid hormone from the androgen group, produced primarily in the Leydig cells of the testes and, to a lesser extent, in the adrenal cortex. It circulates in the blood bound to proteins – mainly sex hormone binding globulin (SHBG) and albumin while only 1–3% remains as “free testosterone,” the biologically active form.
How Testosterone Is Regulated
The hormone’s production is controlled by the hypothalamic–pituitary–gonadal (HPG) axis.
- The hypothalamus secretes gonadotropin-releasing hormone (GnRH).
- The pituitary gland responds by releasing luteinizing hormone (LH).
- LH then stimulates the testes to produce testosterone.
This loop operates via negative feedback: when testosterone rises, GnRH and LH secretion decrease, maintaining hormonal balance.
Factors Affecting Regulation
Multiple factors influence testosterone levels:
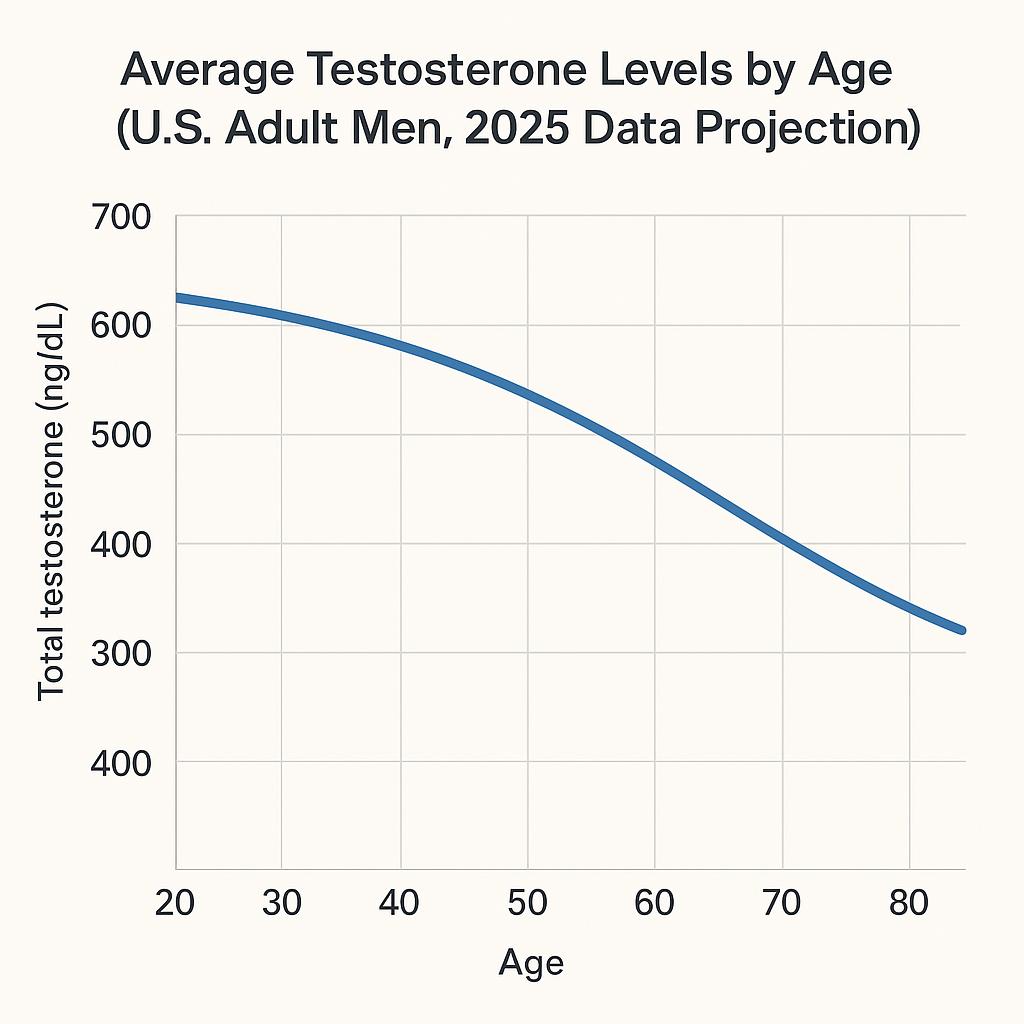
- Age: natural decline begins around age 30 (~1% per year).
- Obesity: excess adipose tissue increases aromatase activity, converting testosterone to estrogen.
- Sleep deprivation: even one week of poor sleep can reduce T levels by up to 10–15%.
- Chronic illness & medications: diabetes, opioids, and glucocorticoids may suppress production.
Age-Related Decline
By age 60, average testosterone levels may be 30–40% lower than in young adulthood. However, not every man experiences symptoms — the concept of “biochemical low T” must be paired with clinical context.
Functions and Health Roles of Testosterone
Puberty and Early Adulthood
During adolescence, testosterone drives the development of secondary sexual characteristics – deepening of the voice, muscle and bone growth, body hair distribution, and sperm production. It also shapes libido and mood regulation.
Adulthood (Ages 20–50)
In adult men, testosterone supports lean muscle mass, bone mineral density, red blood cell production, and sexual desire. It influences metabolic rate and insulin sensitivity. Adequate testosterone helps maintain motivation, cognitive sharpness, and overall vitality.
Later Life (After 50)
As testosterone levels fall, men may experience gradual decreases in strength, bone density, and libido. This process, sometimes referred to as “late-onset hypogonadism,” is often confounded by lifestyle and chronic disease rather than aging alone.
Key Functions of Testosterone Across Age Groups
| Age Group | Primary Roles | Clinical Relevance |
|---|---|---|
| 10–19 | Pubertal development, muscle growth, sperm initiation | Delayed puberty or underdevelopment if deficient |
| 20–39 | Libido, fertility, metabolism, bone density | Peak levels; critical for overall health |
| 40–59 | Maintenance of strength, energy, mental focus | Gradual decline begins |
| 60+ | Bone protection, mood stability | Risk of osteoporosis, fatigue, low libido |
Normal Testosterone Ranges and How to Test Correctly
Reference Ranges in U.S. Men
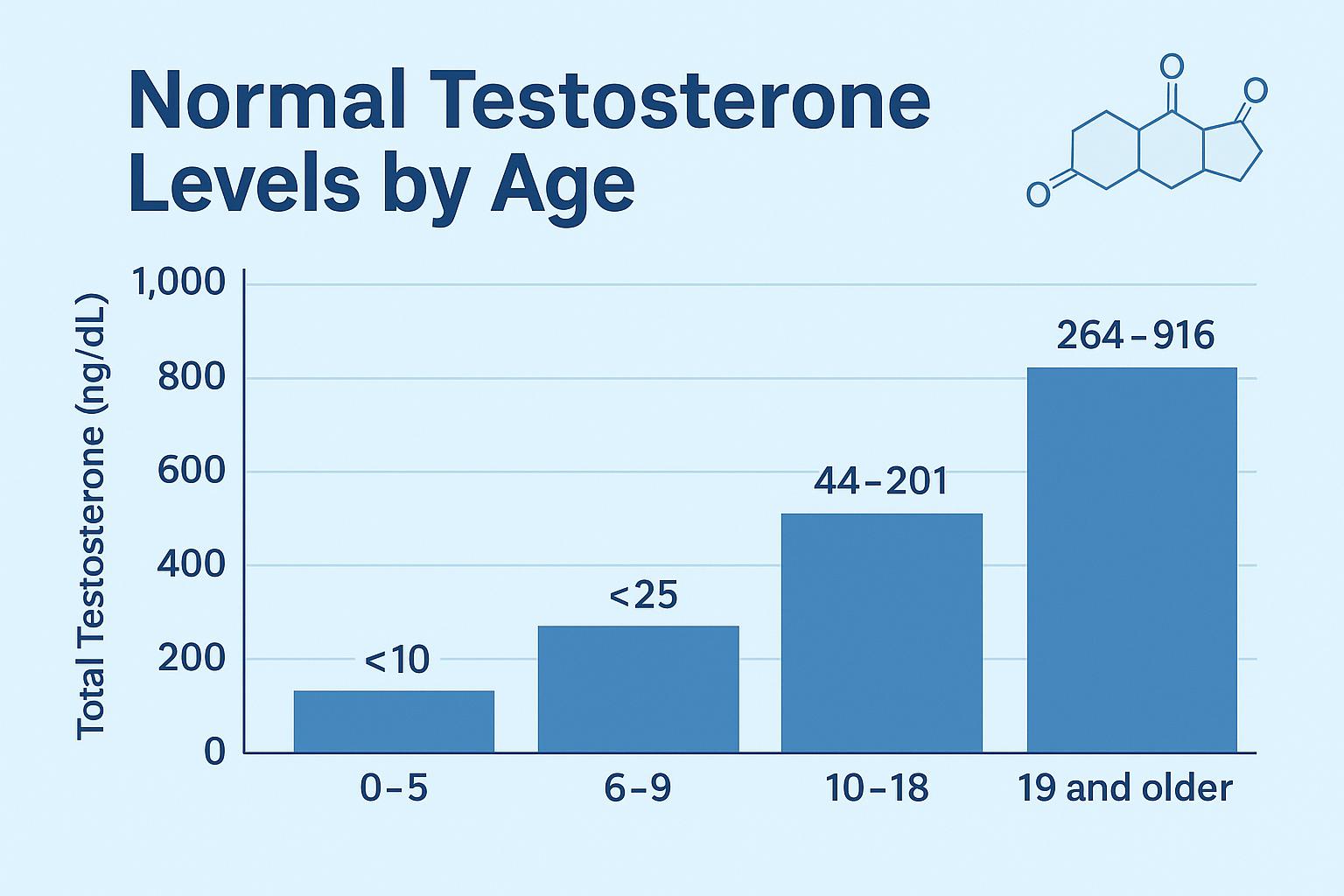
Large-scale studies (Travison et al., J Clin Endocrinol Metab, 2017) define normal total testosterone for healthy men aged 19–39 as 264–916 ng/dL. The American Urological Association (AUA) considers levels below 300 ng/dL as indicative of potential testosterone deficiency when accompanied by symptoms.
Total vs. Free Testosterone
Total testosterone includes both protein-bound and unbound forms. However, conditions that alter SHBG (e.g., obesity, liver disease) can distort total values. Measuring free testosterone via equilibrium dialysis or calculating it based on SHBG levels can improve diagnostic accuracy.
Testing Recommendations
- Timing: Morning sampling (7–10 a.m.), when testosterone peaks.
- Repeat testing: Confirm a low result on at least two separate occasions.
- Pre-analytical factors: Avoid testing during acute illness, fasting is recommended.
- Assay methods: LC-MS/MS is the gold standard; immunoassays may under- or overestimate values.
Common Pitfalls
- Testing too late in the day → falsely low results.
- One-time low reading without symptoms → not diagnostic.
- Lab variability — reference intervals differ slightly between institutions.
Low Testosterone (Male Hypogonadism): Causes, Symptoms, and Management
Low testosterone, also known as male hypogonadism, occurs when the testes produce insufficient amounts of testosterone to maintain normal physiological function. According to the American Urological Association (AUA, 2025), the diagnosis is confirmed when morning testosterone levels are consistently below 300 ng/dL on two separate occasions, accompanied by relevant clinical symptoms.
In clinical practice, low testosterone can arise from two main mechanisms.
- Primary hypogonadism results from testicular dysfunction caused by direct damage for example, trauma, orchitis, chemotherapy, radiation exposure, or congenital genetic conditions such as Klinefelter’s syndrome.
- Secondary hypogonadism originates from inadequate stimulation of the testes by the pituitary or hypothalamus, often due to pituitary tumors, obesity, chronic diseases, high prolactin levels, or medications like opioids and corticosteroids.
- A growing category, functional hypogonadism, describes a reversible suppression of testosterone production due to factors such as severe stress, poor nutrition, or sleep deprivation.
Men with low testosterone often report a gradual loss of vitality rather than a single alarming symptom. Decreased sexual desire, weaker erections, fatigue, mood changes, and reduced muscle mass may all appear subtly over time. Some experience diminished motivation, weight gain, and difficulty maintaining focus. Long-standing deficiency increases the risk of metabolic syndrome, anemia, and osteoporosis, underscoring why accurate diagnosis and management are essential for quality of life.
Diagnostic Approach
Diagnosis begins with detailed clinical evaluation and laboratory confirmation. Blood should be drawn in the early morning (typically between 7 and 10 a.m.) when testosterone peaks. If levels are low, the test is repeated to confirm persistence. Measurement of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin helps distinguish whether the problem lies in the testes or higher in the hypothalamic–pituitary axis. In some cases, imaging such as pituitary MRI is warranted.
The physician must also evaluate for reversible contributors like obesity, poor sleep, alcohol overuse, and chronic illness before considering hormonal therapy.
Clinical Summary Table: Symptoms and Possible Causes of Low Testosterone
| Symptom | Likely Cause | Diagnostic Focus |
|---|---|---|
| Low libido, erectile dysfunction | Aging, obesity, diabetes, medications | Total T, LH, FSH |
| Fatigue, low mood | Sleep apnea, stress, depression | Morning T, thyroid panel |
| Infertility | Pituitary disorder, varicocele | Semen analysis, LH/FSH |
| Muscle loss | Chronic disease, androgen deficiency | Testosterone + body composition |
| Bone fragility | Long-term deficiency | DEXA, vitamin D status |
Elevated Testosterone and Its Clinical Significance
Although public discussion often centers on low testosterone, excessively high levels can also pose health concerns. In adult men not receiving therapy, true hyperandrogenism is rare. Most elevated readings stem from exogenous testosterone use injections, pellets, or anabolic-androgenic steroids obtained without medical supervision. Less frequently, adrenal or testicular tumors may drive overproduction.
Excess testosterone can have paradoxical effects. Initially, men may feel energetic and strong, but over time, excessive androgen levels disrupt normal physiology. Acne, fluid retention, and irritability are common, while suppressed LH and FSH lead to testicular shrinkage and infertility. Increased red-blood-cell production thickens the blood, raising the risk of clotting events such as deep-vein thrombosis. Moreover, chronically high levels can worsen sleep apnea and accelerate prostate growth, leading to urinary symptoms. These outcomes highlight that “more” is not necessarily “better.”
Comparative Overview: Low vs High Testosterone
| Feature | Low T | High T |
|---|---|---|
| Libido | Decreased | Initially high, may later drop |
| Muscle mass | Reduced | Increased but often temporary |
| Fertility | Impaired | Suppressed |
| Mood | Low, apathetic | Irritable, aggressive |
| Hematocrit | Normal/low | Elevated (> 52%) |
| Long-term risk | Osteoporosis, fatigue | Thrombosis, infertility |
Testosterone Replacement Therapy (TRT): Evidence-Based Use
When Therapy Is Indicated
Modern guidelines emphasize that testosterone therapy should be prescribed only for men who have both symptoms and persistently low levels. Treatment is not intended for age-related “optimization” or bodybuilding enhancement. Once reversible causes are addressed, properly selected patients may benefit from hormonal replacement under specialist supervision.
TRT is contraindicated in men with active prostate or breast cancer, severe erythrocytosis, uncontrolled sleep apnea, or those planning to conceive, since exogenous testosterone suppresses sperm production. Physicians typically discuss fertility-preserving alternatives such as clomiphene citrate or gonadotropins before starting lifelong therapy.
Treatment Modalities
Several formulations allow for individualized therapy:
| Form | Dosing Route | Advantages | Drawbacks |
|---|---|---|---|
| Topical gels/creams | Daily skin application | Convenient, steady absorption | Skin contact risk, variable levels |
| Transdermal patches | Applied nightly | Physiologic rhythm | Skin irritation |
| Intramuscular injections | Every 1–2 weeks | Predictable dose, affordable | Peaks and troughs, self-injection |
| Subcutaneous pellets | Implanted 3–6 months | Long-acting | Minor surgical procedure |
| Oral testosterone undecanoate | 200–400 mg daily | Convenient, no needles | Variable absorption, liver monitoring |
Monitoring and Safety
Therapy demands continuous evaluation. Hormone levels, hematocrit, and prostate-specific antigen (PSA) are checked after three to six months and annually thereafter. The therapeutic goal is to maintain testosterone within the mid-normal range (400–700 ng/dL) enough to relieve symptoms but below the threshold that increases cardiovascular or hematologic risks.
Recent clinical trials, including the TRAVERSE Study (2023) and follow-up reports in The New England Journal of Medicine (2024), suggest that appropriately monitored TRT does not raise cardiovascular event rates in men with bona fide hypogonadism. Nevertheless, unsupervised “boosting” through unregulated clinics or online products remains dangerous, often leading to overdosing, infertility, and hormone withdrawal crises once treatment stops.
Monitoring and managing side effects during testosterone replacement therapy
Evidence-Based Natural Strategies to Support Testosterone
Before considering testosterone therapy, physicians emphasize the importance of lifestyle changes. Multiple studies confirm that healthy habits can naturally increase testosterone by 10–30%, especially in men with mild or functional deficiency.
A balanced diet supports hormone synthesis. Testosterone is derived from cholesterol, so extreme low-fat diets can impair production. Nutrient-rich foods such as eggs, fish, olive oil, nuts, and leafy greens provide essential building blocks. Micronutrients like zinc, magnesium, and vitamin D also play key roles in steroid hormone metabolism.
Regular resistance exercise remains one of the most effective nonpharmacologic ways to elevate testosterone. Strength training three to four times a week, with adequate rest between sessions, improves both total and free testosterone levels. Excessive endurance training, however, may have the opposite effect by raising cortisol and suppressing the hypothalamic pituitary–gonadal axis.
Sleep is another fundamental factor. Testosterone secretion peaks during the early hours of the morning, closely tied to REM sleep. Men sleeping fewer than six hours per night can have up to 20% lower testosterone. Prioritizing seven to eight hours of quality rest helps restore hormonal rhythm.
Maintaining healthy body composition significantly affects testosterone levels. Adipose tissue, particularly visceral fat, contains aromatase, an enzyme that converts testosterone into estrogen. Even modest weight reduction (5–10%) often normalizes hormone levels in obese men.
Finally, stress management is crucial. Chronic psychological stress increases cortisol, which suppresses testosterone. Mindfulness, resistance training, balanced workload, and social connection all contribute to better endocrine health.
When to See a Doctor
Men should seek medical evaluation when they experience persistent fatigue, low libido, erectile dysfunction, infertility, mood changes, or unexplained muscle and bone loss. These symptoms are not always caused by testosterone deficiency, but they warrant assessment by a healthcare professional.
At a consultation, an endocrinologist or urologist typically conducts a detailed history, physical exam, and laboratory testing. This process helps differentiate true hypogonadism from other conditions such as thyroid disorders, depression, or medication effects. Testing should never be based solely on curiosity or age; it should be guided by symptoms and clinical evidence.
Conclusion
Testosterone plays a vital role in men’s overall health, influencing physical strength, sexual function, mood, and metabolism. While age-related decline is natural, significant or symptomatic deficiency deserves medical attention – not self-treatment.
The safest path to hormonal balance combines lifestyle optimization, professional evaluation, and evidence-based therapy when indicated. Natural approaches like exercise, sleep, and weight control are often sufficient for mild cases. When medication is necessary, supervised testosterone replacement therapy (TRT) can be both safe and effective if monitored correctly.
Every man should aim for a balanced, not maximal, testosterone level – one that supports vitality, clarity, and long-term health without unnecessary risks.
Frequently Asked Questions (FAQ)
What is a normal testosterone level for men in the United States?
For healthy adult men aged 19–39, total testosterone typically ranges between 264 and 916 ng/dL. Levels below 300 ng/dL with symptoms may indicate testosterone deficiency.
How early should blood be drawn for testosterone testing?
The optimal time is between 7 a.m. and 10 a.m., when testosterone peaks naturally. Testing should always be repeated for confirmation.
Can lifestyle changes really increase testosterone naturally?
Yes. Exercise, proper nutrition, adequate sleep, and stress management can improve testosterone by up to 30% in men with mild deficiency.
When is testosterone therapy appropriate?
TRT is prescribed only to men with symptoms and confirmed low levels, after reversible causes (obesity, illness, medication) are ruled out.
What are the main risks of testosterone therapy?
Potential risks include increased hematocrit, acne, reduced fertility, and fluid retention. These effects are minimized through medical supervision.
How long does it take for testosterone therapy to work?
Most men notice improvements in libido and mood within 4–6 weeks, while changes in body composition and bone density appear after 3–6 months.
References
- American Urological Association (AUA) – Testosterone Deficiency Guideline (2025)
- Endocrine Society – Testosterone Therapy in Men with Hypogonadism: Clinical Practice Guideline (2024 update)
- CDC – National Health and Nutrition Examination Survey (NHANES)
- Cardiovascular Safety of Testosterone-Replacement Therapy – randomized noninferiority trial of TRT in men with hypogonadism and cardiovascular risk
- Testosterone Therapy in Older Men: Present and Future – review of recent RCTs on TRT in older men (2025)
