Psychological erectile dysfunction (ED), also known as psychogenic erectile dysfunction, is one of the most common forms of sexual dysfunction in men under 40 and a growing concern across all age groups in 2025. Unlike organic ED, which is caused by vascular, neurological, or hormonal problems, psychological ED is primarily driven by mental health and emotional factors such as stress, anxiety, and depression.
Understanding the root causes and modern approaches to treatment is essential not only for restoring sexual health but also for improving overall well-being.
How Stress and Anxiety Impact Erections
Sexual performance depends on a delicate balance between the brain, nervous system, blood vessels, and hormones. Stress and anxiety disrupt this balance in multiple ways:
- Fight-or-flight response: When the brain perceives stress, it triggers adrenaline release, which constricts blood vessels and makes erections harder to achieve or maintain.
- Performance anxiety: Men may worry about their ability to perform sexually, creating a self-fulfilling cycle where fear leads to failure, which reinforces more fear.
- Chronic stress: Prolonged psychological strain contributes to sleep disturbances, hormonal imbalances, and reduced libido, further worsening erectile function.
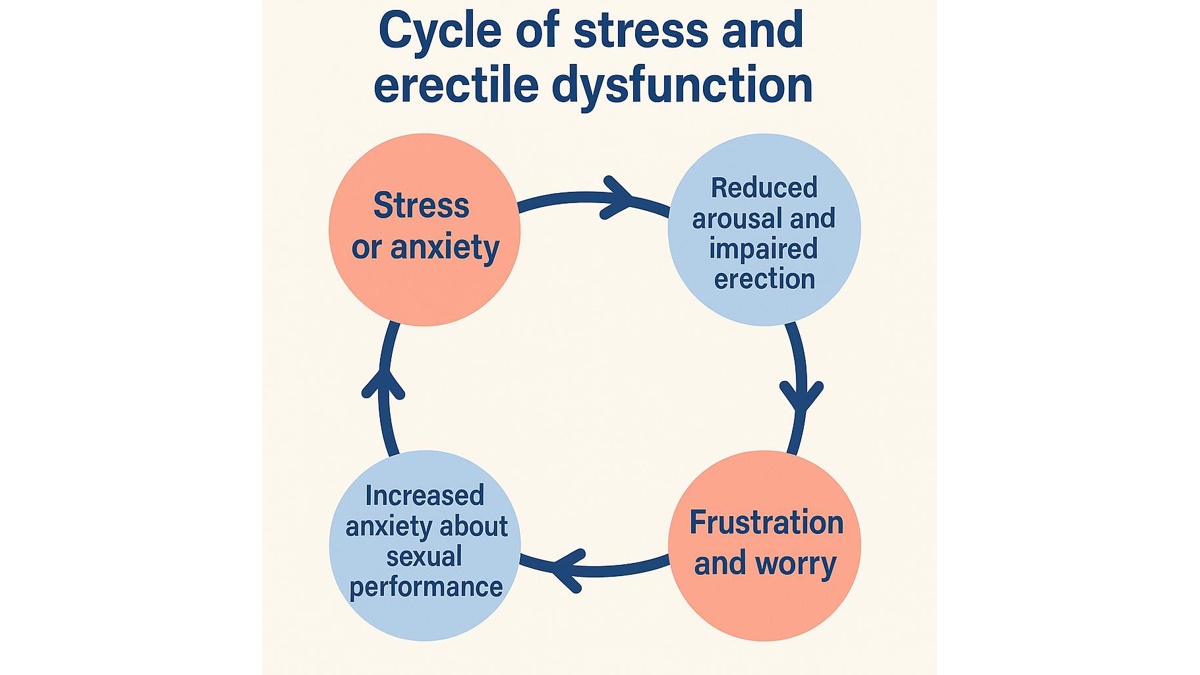
This vicious loop often keeps men trapped unless properly addressed through therapy and structured interventions.
For a broader perspective on myths surrounding erectile dysfunction, see Erectile Dysfunction: Myths vs Facts.
How Doctors Diagnose Psychogenic ED
Accurate diagnosis is the cornerstone of successful treatment. Since erectile dysfunction may result from multiple overlapping causes, distinguishing psychogenic erectile dysfunction from organic conditions is critical. In 2025, physicians follow a step-by-step process that integrates both psychological and physical assessment tools.
Comprehensive patient history
Doctors begin with an in-depth interview covering:
- Onset and pattern: Psychogenic ED often develops suddenly, sometimes after a stressful event or in new relationships. In contrast, organic ED usually progresses gradually over months or years.
- Situational factors: Men with psychological ED may experience dysfunction only in certain contexts—for example, with a new partner or under stress—while spontaneous or solo erections remain normal.
- Relationship dynamics: Conflict, lack of intimacy, or unresolved emotional issues are strong predictors of stress-related ED.
- Lifestyle and habits: Sleep deprivation, overwork, alcohol, and recreational drug use are assessed, since they often exacerbate anxiety and reduce libido.
Psychological screening tools
Validated questionnaires help quantify the role of stress and anxiety:
- IIEF-5 (International Index of Erectile Function) – measures severity and frequency of ED.
- DASS-21 (Depression, Anxiety, Stress Scale) – identifies depression, anxiety, and stress as contributors.
- Sexual Performance Anxiety Scale (SPAS) – evaluates fear and anxiety around sexual activity.
These instruments not only confirm psychogenic causes but also track treatment progress.
Physical and laboratory evaluation
Even when psychological ED is suspected, clinicians exclude organic factors such as diabetes, vascular disease, and low testosterone. Typical tests include:
- Blood pressure and cardiovascular assessment.
- Hormone panel (testosterone, prolactin, thyroid hormones).
- Glucose and lipid profile for metabolic health.
Nocturnal penile tumescence (NPT) testing
Men with psychogenic ED usually demonstrate normal nighttime erections, while men with organic causes often do not. In 2025, wearable technology and home-based monitoring provide more patient-friendly alternatives to traditional lab testing.
Advanced digital diagnostics
Modern innovations enhance accuracy:
- Wearable erection monitors track duration and rigidity during sleep.
- AI-based diagnostic algorithms analyze patterns of anxiety, erection quality, and lifestyle to suggest likely psychogenic vs. organic origin.
- Telehealth assessments allow integration of self-reported psychological data with wearable results.
Red flags for psychogenic ED
- Sudden onset in an otherwise healthy man.
- Normal erections during masturbation or sleep but not with a partner.
- Strong association with stressful events or relationship issues.
- Absence of vascular or hormonal abnormalities on testing.
Comparison: Psychogenic vs. Organic ED
| Feature | Psychogenic ED | Organic ED |
| Onset | Sudden, often linked to stress or specific situations | Gradual, progressive over months or years |
| Age group | More common in younger men (<40) | Increases with age (>50) |
| Triggers | Stress, anxiety, depression, relationship conflict | Vascular disease, diabetes, hormonal deficiency, nerve damage |
| Morning erections | Usually preserved | Often reduced or absent |
| Situational patterns | Occurs with partner, but not alone | Consistent across all settings |
| Diagnostic tests | Normal hormone levels, normal NPT, psychological screening abnormal | Abnormal vascular studies, low testosterone, impaired NPT |
Multidisciplinary evaluation
The gold standard in 2025 is a team-based approach: urologists ensure organic causes are excluded, psychologists assess mental health, and sex therapists address performance anxiety. This holistic method prevents misdiagnosis and improves long-term treatment success.
Effective Psychological Therapies for Psychogenic Erectile Dysfunction in 2025
In modern clinical practice, it is common for men to experience more than one psychogenic sexual disorder at the same time. For example, premature ejaculation often coexists with erectile difficulties, since both conditions are strongly influenced by performance anxiety, stress, and negative thought patterns. The encouraging news is that the same therapeutic tools such as CBT, sex therapy, and mindfulness are effective for both. For men interested in exploring this topic further, we recommend our detailed guide on Premature Ejaculation: Causes, Diagnosis, and Modern Treatment Options.
This overlap demonstrates why therapy must address the full psychological landscape rather than focusing on erections alone. A man who learns to manage stress and anxiety through therapy typically sees improvement across multiple aspects of his sexual life, not just erectile function.
Cognitive Behavioral Therapy (CBT)
One of the most widely studied approaches is CBT. This method helps patients recognize destructive thought patterns such as “I will fail again” or “I am not attractive enough” and replace them with more constructive perspectives. Modern CBT sessions often integrate digital platforms, allowing men to access therapy remotely. Clinical studies demonstrate that patients who undergo CBT not only regain erectile function but also report improved self-esteem and reduced anxiety in daily life.
Sex therapy
Sex therapy also plays a vital role. It goes beyond individual treatment and involves the partner, addressing relational dynamics that often worsen erectile problems. Therapists use techniques like sensate focus, which encourages couples to rebuild intimacy without the immediate pressure of penetration. This step-by-step method reduces anxiety, strengthens emotional bonds, and helps restore natural erectile responses.
Mindfulness-based therapy
Another promising direction is mindfulness-based therapy. Mindfulness practices such as meditation, yoga, and controlled breathing reduce the body’s stress response, helping men stay present instead of worrying about performance. Clinical evidence from 2023–2025 shows that combining mindfulness with CBT leads to significantly higher patient satisfaction compared to either therapy alone.
Medication Support: How PDE5 Inhibitors Help in Psychological erectile Dysfunction
While psychotherapy is essential, many men with psychological erectile dysfunction benefit from temporary use of medication. Drugs like sildenafil and tadalafil, known as PDE5 inhibitors, do not treat the underlying psychological cause, but they often reduce performance anxiety. A man who has failed in the past may feel more confident knowing he has medical support. This restored confidence allows therapy to progress more effectively.
In some cases, when ED is linked to depression or generalized anxiety disorder, psychiatrists may prescribe antidepressants or anxiolytics. However, these require careful monitoring, since certain antidepressants can worsen sexual function. Fortunately, in 2025 newer-generation antidepressants with minimal sexual side effects are available, offering safer options for patients who need both mental health and sexual health support.
Key Differences in Treating Psychogenic vs Organic Erectile Dysfunction
Doctors emphasize that treatment strategies differ dramatically depending on whether the ED is primarily psychological or organic. The table below summarizes these differences:
| Aspect | Psychogenic Erectile Dysfunction | Organic Erectile Dysfunction |
| Primary cause | Stress, anxiety, depression, relationship problems | Vascular disease, diabetes, hormonal imbalance, neurological damage |
| Main treatment | Psychotherapy (CBT, sex therapy, mindfulness), occasional PDE5 support | PDE5 inhibitors, hormonal therapy, surgery, vascular treatment |
| Role of medication | Supportive, not curative | Often the mainstay of treatment |
| Prognosis | Very favorable with combined therapy and lifestyle change | Depends on severity of underlying condition |
This comparison highlights why accurate diagnosis is essential: a man with psychological ED may recover completely through therapy and stress reduction, while a man with vascular disease may need lifelong medication.
Lifestyle Strategies for Long-Term Results in Psychological ED
Psychological erectile dysfunction is not simply a mental condition it is deeply tied to overall health and lifestyle. By 2025, doctors emphasize that managing stress and ED requires a holistic approach that goes far beyond therapy sessions or medications.
One of the most significant factors is sleep quality. Men who regularly get fewer than six hours of sleep per night have higher rates of ED, largely due to increased cortisol levels and reduced testosterone production. Restorative sleep not only enhances energy and mood but also restores natural sexual responsiveness.
Nutrition also plays a critical role. Diets rich in antioxidants, omega-3 fatty acids, and whole foods improve vascular health and reduce inflammation, indirectly benefiting erectile function. Excessive processed food, sugar, and alcohol, on the other hand, fuel anxiety and lower libido.
Physical activity serves as a natural antidepressant. Regular aerobic and strength training reduce stress hormones and improve blood circulation, both essential for healthy erections. Moreover, exercise builds self-confidence, which helps break the cycle of performance anxiety.
Finally, lifestyle adjustments should target stress management. Techniques such as yoga, journaling, and mindfulness meditation not only lower baseline anxiety but also enhance body awareness and sexual satisfaction. As highlighted in our resource How Lifestyle Affects Erectile Function, even small, consistent changes — better diet, improved sleep, and stress reduction – can yield long-term benefits for men with psychogenic erectile dysfunction.
When to See a Doctor About Psychogenic Erectile Dysfunction
Many men hesitate to consult a doctor about ED, especially when they suspect the cause is psychological. Yet delaying professional help often prolongs the condition and increases anxiety. In 2025, experts recommend seeking medical advice if:
- Erectile dysfunction has persisted for longer than three months, even if situational.
- Symptoms are accompanied by severe stress, anxiety, or depression that affect daily life.
- There is a significant impact on relationships or self-esteem.
- The partner’s age is over 35 and fertility is a concern, since combined evaluation may be needed.
- There are any “red flags,” such as reduced libido, pain, penile curvature, or other symptoms suggesting an organic condition.
Doctors can quickly distinguish between psychogenic and organic erectile dysfunction, ensuring that men receive the correct therapy without unnecessary medications.
Frequently Asked Questions (FAQ)
Can stress alone cause erectile dysfunction?
Yes, chronic stress and anxiety can cause psychological erectile dysfunction by disrupting the nervous system and blood flow. Over time, this creates a cycle of fear and repeated erectile problems.
How do I know if my erectile dysfunction is psychological?
If you have normal erections during sleep or masturbation but struggle with a partner, it is likely psychogenic erectile dysfunction. Doctors confirm this through medical history, psychological screening, and nocturnal erection testing.
Do PDE5 inhibitors help with psychological erectile dysfunction?
They can help by boosting confidence and reducing performance anxiety. However, they do not treat the root psychological causes, so therapy is usually needed.
Can therapy permanently cure psychogenic erectile dysfunction?
Yes, therapies like CBT, sex therapy, and mindfulness often restore sexual function completely. Combining therapy with lifestyle improvements gives the best long-term results.
What if I have both psychological and physical erectile dysfunction?
Many men experience mixed erectile dysfunction, where stress adds to vascular or hormonal issues. In these cases, treatment combines medical therapy with psychological support.
Is psychological erectile dysfunction common in young men?
Yes, men under 40 often develop psychogenic erectile dysfunction due to stress, performance anxiety, or relationship problems. Fortunately, the condition responds very well to therapy and stress management.
References
- American Psychological Association: evidence-based treatments for sexual problems, including psychological erectile dysfunction
- Mayo Clinic: overview of erectile dysfunction with focus on psychological causes
- PubMed: recent review on psychogenic erectile dysfunction management and mental health factors
- Cleveland Clinic: clinical guide to erectile dysfunction, diagnosis, and mental health links
- Harvard Health: how stress impacts sexual health and erectile function
