Prostatitis Treatment in 2025: What’s New?
Prostatitis is one of the most common urological conditions in men and, as of 2025, remains a significant clinical and social concern. According to the NIH, up to 10–15% of men will experience prostatitis symptoms during their lifetime, and in many cases the condition becomes chronic.
Modern research highlights that chronic prostatitis affects far more than the prostate itself. Men living with this condition often experience chronic pelvic pain, urinary dysfunction, reduced sexual function, and psychological distress. Quality of life studies consistently rank chronic prostatitis as having a burden similar to conditions such as congestive heart failure or Crohn’s disease.
Because of this, urology has shifted its focus in the past decade: instead of merely suppressing symptoms, the emphasis is now on innovative diagnostics and personalized therapies that address both the bacterial and non-bacterial forms of prostatitis. In this article, we will explore what’s new in diagnosis, pharmacological therapy, physiotherapy, and research innovations for prostatitis treatment in 2025.
Updated Diagnostic Tools
Effective prostatitis treatment begins with accurate diagnosis. For decades, clinicians relied on symptom descriptions, physical exams, and basic urine cultures. While these remain important, the diagnostic toolbox in 2025 has expanded dramatically, driven by imaging advances, molecular biology, and artificial intelligence.
Modern diagnostic tools now include:
- Multiparametric ultrasound (mpUS): High-resolution imaging to detect areas of inflammation and structural abnormalities within the prostate.
- Magnetic resonance imaging (MRI): Used not only to differentiate prostatitis from prostate cancer or benign prostatic hyperplasia but also to assess treatment response over time.
- Next-generation microbiological testing: PCR assays and genetic sequencing to detect hidden infections and bacterial biofilms that standard cultures may miss.
- Biomarkers of inflammation: Measured in blood, urine, and seminal fluid, helping stratify disease severity and guide targeted therapy.
- Digital health tools: Mobile apps allow patients to track symptoms, while AI algorithms analyze large datasets to support more accurate classification between bacterial and non-bacterial chronic prostatitis.
Diagnostic Pathway for Prostatitis
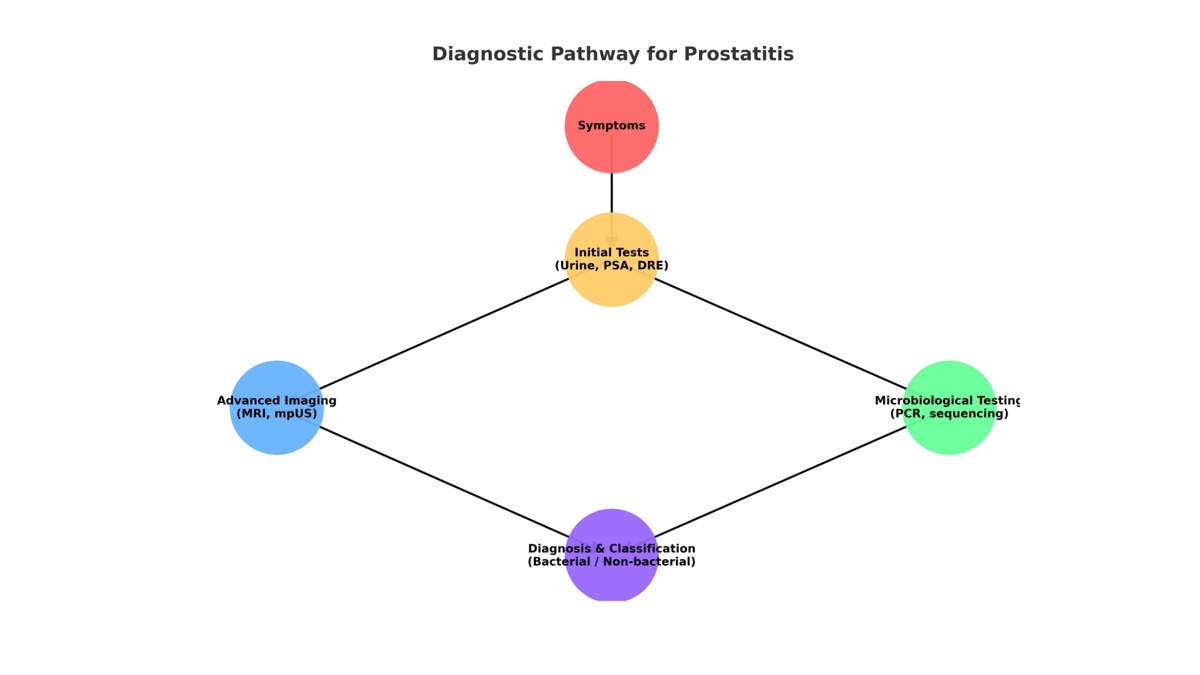
Unlike in earlier years, diagnosis today recognizes the multifactorial nature of chronic prostatitis. It is not always a simple bacterial infection. Instead, immune dysfunction, nerve sensitization, and even alterations in the urinary and seminal microbiome often play a role. Understanding these mechanisms allows for more individualized and effective prostatitis therapy.
To learn more about the background and subtypes of this condition, see Prostatitis overview.
Advanced Antibiotics and Anti-inflammatory Drugs
Antibiotics remain the foundation of treatment for acute bacterial prostatitis, but their role in chronic prostatitis is far more nuanced. In 2025, prescribing patterns reflect concerns over antibiotic resistance as well as an improved understanding of drug delivery into prostate tissue.
Antibiotic innovations include:
- Next-generation fluoroquinolones with better prostate penetration and a safer side-effect profile.
- Combination regimens with biofilm-disrupting agents, designed to break down bacterial shields and improve eradication rates.
- Personalized antibiotic strategies, guided by molecular diagnostics and local resistance data, which reduce unnecessary long-term exposure.
For men with chronic non-bacterial prostatitis, however, antibiotics show limited benefit. Instead, anti-inflammatory therapy plays a central role. Nonsteroidal anti-inflammatory drugs (NSAIDs) remain widely used, but recent years have introduced more selective COX-2 inhibitors and immune-modulating agents that target specific inflammatory pathways.
In addition, alpha-blockers continue to be prescribed to improve urinary flow and reduce pelvic pain in selected patients, especially those with significant lower urinary tract symptoms.
Key point: Antibiotics are most effective in acute bacterial prostatitis, while chronic forms increasingly require a combination of anti-inflammatory medications, pain management, and non-pharmacological strategies.
Modern Physiotherapy: Laser, Shockwave, and Magnetotherapy
While antibiotics and anti-inflammatory medications remain important, physiotherapy has gained increasing recognition as a central component of chronic prostatitis treatment. In 2025, novel technologies allow urologists to address both inflammation and pelvic pain more effectively.
Laser therapy has become a standard adjunct in many specialized centers. Low-level laser irradiation applied transperineally or rectally improves microcirculation, reduces inflammatory mediators, and promotes healing of prostatic tissue. Clinical trials between 2022 and 2025 report that men receiving laser therapy in combination with medication achieve significantly higher symptom relief scores compared to those treated with drugs alone.
Shockwave therapy (also known as extracorporeal shockwave therapy, ESWT) is another promising modality. Originally used for erectile dysfunction and kidney stones, shockwave therapy is now applied at low intensities to the prostate and surrounding pelvic floor muscles. Studies indicate it reduces chronic pelvic pain, improves blood flow, and modulates nerve hypersensitivity – one of the key drivers of chronic prostatitis symptoms.
Magnetotherapy uses pulsed magnetic fields to enhance tissue repair and reduce muscle tension. While evidence is still emerging, early trials show benefits in pain reduction and urinary function. Importantly, this modality is non-invasive, painless, and well tolerated, making it an attractive option for patients seeking drug-free management strategies.
Comparison of physiotherapy methods
| Physiotherapy Method | Mechanism of Action | Reported Effectiveness (2023–2025) | Side Effects |
|---|---|---|---|
| Laser therapy | Improves blood flow, reduces inflammatory markers | Moderate-to-high symptom relief when combined with medication | Minimal (mild local warmth) |
| Shockwave therapy (ESWT) | Enhances microcirculation, reduces nerve hypersensitivity | Significant reduction in pelvic pain and improved QoL | Mild discomfort during session |
| Magnetotherapy | Promotes tissue repair, relaxes pelvic floor | Early studies show promising pain reduction | None significant, very safe |
In clinical practice, physiotherapy is rarely used alone. Instead, it is part of a multimodal prostatitis therapy strategy that combines medication, physical rehabilitation, and patient education.
Physiotherapy also intersects with sexual health rehabilitation. In cases where prostatitis has contributed to erectile dysfunction, clinicians may recommend additional supportive technologies such as : vacuum erection devices (VEDs) to restore confidence and improve sexual function.
Alternative and Experimental Treatments
Alongside mainstream therapies, researchers continue to investigate alternative and experimental methods to broaden the scope of prostatitis treatment.
One area of growing interest is phytotherapy and nutraceuticals. Extracts such as quercetin, pollen extract, and saw palmetto have been studied for their anti-inflammatory and antioxidant effects. While not replacements for antibiotics, these agents can complement traditional treatments and help reduce flare-ups of chronic symptoms.
Probiotics are another exciting area of investigation. As scientists better understand the relationship between the urinary microbiome and prostate health, targeted probiotics may help restore a healthy microbial balance and reduce recurrent inflammation.
On the experimental frontier, stem cell therapy is attracting attention. Early clinical trials are exploring whether mesenchymal stem cells can regenerate damaged prostatic tissue and modulate immune responses. Though still in the experimental stage, this approach offers hope for patients with refractory cases of chronic prostatitis.
Finally, novel biologic therapies – including monoclonal antibodies against specific inflammatory mediators – are being tested in clinical trials. These could represent a breakthrough for patients with chronic pelvic pain syndrome, particularly those who do not respond to current medications.
Key takeaway: Alternative and experimental treatments are not yet part of routine clinical care, but they highlight the potential for future breakthroughs. Patients should only consider these options under medical supervision, ideally within structured clinical trials.
How Prostatitis Affects Sexual Health
Prostatitis is more than an inflammatory disease of the prostate it has profound implications for men’s sexual well-being. Clinical surveys consistently show that erectile dysfunction (ED), premature ejaculation, and decreased libido are more common among men with chronic prostatitis than in the general population.
The connection is multifactorial. Chronic inflammation alters blood flow and nerve sensitivity in the pelvic region, directly impairing erectile function. Pain during or after ejaculation is a hallmark symptom of chronic prostatitis and can condition men to avoid sexual activity. In addition, the psychological burden stress, anxiety, and reduced self-confidence further exacerbates sexual dysfunction.
Long-term, untreated prostatitis may contribute to reduced semen quality, which can complicate fertility outcomes. While not all men with prostatitis experience infertility, studies suggest that recurrent or severe cases can lower sperm motility and increase oxidative stress in seminal fluid.
Effective prostatitis therapy therefore goes beyond infection control; it must also address sexual health. Urologists increasingly integrate pelvic floor physiotherapy, medications for ED, and supportive interventions to restore intimacy.
Differential diagnosis is also crucial. Conditions such as ссылка: benign prostatic hyperplasia often overlap with prostatitis symptoms and can independently contribute to sexual problems. A clear diagnosis ensures that men receive tailored therapy for both conditions.
Research and Future Directions
The treatment landscape for prostatitis is evolving rapidly. Between 2023 and 2025, several new areas of research have emerged that could transform how clinicians manage this complex condition.
- Microbiome-based therapies: Ongoing studies explore the relationship between urinary and seminal microbiota and chronic prostatitis. The development of personalized probiotics and targeted antimicrobials may offer safer long-term control of inflammation.
- Regenerative medicine: Stem cell therapy, though still experimental, is gaining traction. Trials suggest that stem cells may repair damaged prostatic tissue, reduce fibrosis, and reset abnormal immune responses.
- Precision medicine: Genetic profiling of patients could help identify subgroups of men with specific inflammatory or neurological pathways driving their symptoms. Tailored therapies – for example, biologics targeting TNF-alpha or IL-1 – are under consideration.
- Digital health integration: Mobile health apps for symptom tracking, telemedicine consultations, and AI-based treatment recommendations are increasingly adopted. These technologies shorten diagnostic delays and enhance long-term monitoring.
- Multimodal treatment frameworks: The future standard of care will likely combine advanced pharmacology, physiotherapy, lifestyle modification, and digital monitoring, creating a holistic patient-centered approach.
Prostatitis in 2025: Key Takeaways
By 2025, prostatitis treatment has entered a new era. Modern diagnostics – including MRI, advanced microbiological testing, and biomarker analysis – allow clinicians to pinpoint the underlying causes more accurately than ever before. Pharmacological therapy is more personalized, physiotherapy offers tangible relief, and emerging fields like regenerative medicine promise entirely new possibilities.
Importantly, clinicians now view prostatitis as a condition with systemic consequences – not only a localized inflammation. Its impact on sexual health, mental well-being, and quality of life requires a holistic management plan.
For men living with chronic prostatitis, the message is clear: there is more hope in 2025 than ever before. With innovative treatments, lifestyle strategies, and ongoing research, long-term symptom relief and improved sexual health are achievable goals.
Frequently Asked Questions (FAQ)
How common is prostatitis?
According to the NIH, prostatitis affects 10–15% of men at some point in their lives, making it one of the most prevalent urological diagnoses.
Can chronic prostatitis be cured?
Acute bacterial prostatitis can often be cured with antibiotics. Chronic prostatitis, however, is usually a long-term condition. While a complete cure is rare, modern treatments in 2025 significantly reduce symptoms and improve quality of life.
What is the role of physiotherapy in prostatitis therapy?
Techniques such as laser therapy, shockwave therapy, and magnetotherapy have shown measurable benefits in reducing pain and improving urinary function, especially when combined with medication.
How does prostatitis impact sexual health?
Men with chronic prostatitis are more likely to experience erectile dysfunction, reduced libido, and painful ejaculation. Addressing sexual health is now considered an integral part of prostatitis treatment.
When should I see a urologist?
Men should consult a urologist if they experience persistent pelvic pain, urinary difficulties, or sexual dysfunction lasting more than a few weeks. Early diagnosis leads to more effective therapy and prevents long-term complications.
References
- NIDDK – Prostatitis (Inflammation of the Prostate)
- European Association of Urology – Prostatitis Guidelines 2024
- Mayo Clinic – Prostatitis: Diagnosis and treatment
- Cleveland Clinic – Prostatitis overview
- PubMed – A Review of Current Treatments for Chronic Prostatitis
- PubMed – Male Chronic Pelvic Pain: AUA Guideline: Part II Treatment
