The connection between diabetes and erectile dysfunction is now firmly established in scientific literature. High blood sugar levels damage blood vessels and nerves, both of which are critical for normal erectile function. As a result, men with diabetes face a much higher risk of developing ED compared to the general population. The good news is that with proper management medical treatment, lifestyle changes, and preventive care potency can be preserved even in the presence of chronic disease.
This article explores in detail how diabetes impacts sexual health in men, what treatment options are available in 2025, and which preventive strategies offer the strongest evidence for protecting sexual function.
How Diabetes Affects Erectile Function?
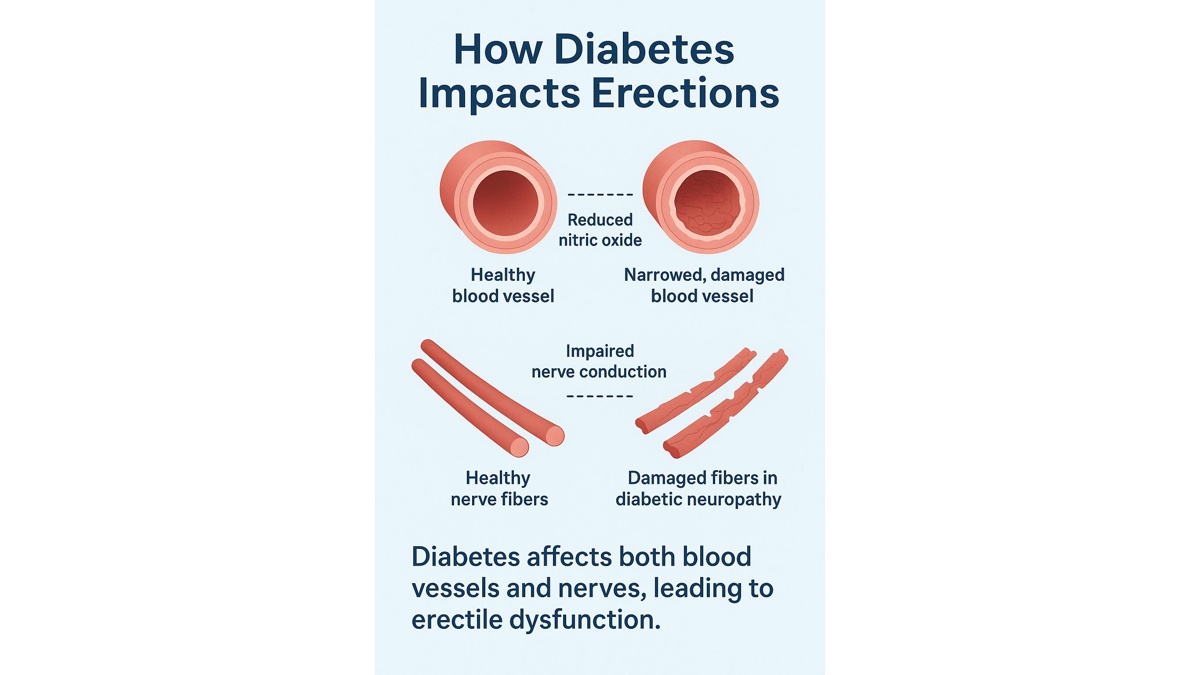
An erection is a complex physiological process involving blood vessels, nerves, hormones, and psychological factors. Diabetes disrupts this delicate system in two primary ways:
Vascular damage (endothelial dysfunction)
Chronic hyperglycemia damages the inner lining of blood vessels (endothelium). This reduces the ability to produce nitric oxide, a molecule essential for blood vessel relaxation. Without sufficient nitric oxide, blood flow to the penis is restricted, making it difficult to achieve or maintain an erection.
Neurological damage (diabetic neuropathy)
Diabetes also affects peripheral nerves. Over time, high glucose levels impair nerve conduction, leading to decreased penile sensitivity and weaker neural signaling to trigger erections. Neuropathy can also disrupt the autonomic nervous system, which regulates involuntary functions such as vascular tone.
The combination of vascular and neurological impairment makes erectile dysfunction in men with diabetes particularly challenging to treat compared to ED of purely psychogenic origin.
Risk of Erectile Dysfunction in Men with Diabetes
Multiple large cohort studies and meta-analyses confirm that men with diabetes are two to three times more likely to experience erectile dysfunction compared to men without the disease. According to the American Diabetes Association (ADA), erectile dysfunction affects up to 50–75% of men with type 2 diabetes at some point in their lives.
The risk is influenced by several factors:
- Duration of diabetes: The longer a man lives with uncontrolled diabetes, the higher the likelihood of vascular and neurological complications.
- Glycemic control: Poor HbA1c levels are strongly associated with ED.
- Age: Older men with diabetes face compounded risk from both aging and metabolic disease.
- Comorbidities: Hypertension, dyslipidemia, obesity, and cardiovascular disease further increase the risk.
It is also important to note that ED can be an early marker of undiagnosed diabetes. Men presenting with new-onset erectile difficulties should be evaluated for metabolic disorders, as vascular dysfunction often appears before overt symptoms of diabetes.
Treatment Options in 2025
Management of erectile dysfunction in men with diabetes requires a personalized approach, as both vascular and neurological damage complicate therapy. By 2025, urology guidelines emphasize combining pharmacological treatments, hormone therapy, and device-based solutions.
PDE5 inhibitors – first-line therapy
Phosphodiesterase-5 inhibitors remain the cornerstone of ED treatment in men with diabetes. They enhance nitric oxide signaling and improve penile blood flow. The most commonly prescribed are:
- Sildenafil (Viagra): Short-acting, typically taken 30–60 minutes before intercourse.
- Tadalafil (Cialis): Long-acting, effective up to 36 hours, also available in low-dose daily regimens.
- Vardenafil (Levitra, Staxyn): Similar to sildenafil, with rapid onset.
- Avanafil (Stendra): Faster onset, often better tolerated in men with cardiovascular comorbidities.
Although men with diabetes may respond slightly less effectively compared to the general population, PDE5 inhibitors still provide significant improvement for most patients.
Testosterone replacement therapy (TRT)
Hypogonadism (low testosterone) is prevalent in men with type 2 diabetes. When confirmed through laboratory testing, TRT can improve libido and enhance the efficacy of PDE5 inhibitors. Options include topical gels, intramuscular injections, and long-acting implants. Regular monitoring of prostate health, hematocrit, and cardiovascular risk is essential.
Vacuum erection devices (VEDs)
VEDs create negative pressure that draws blood into the penis, followed by placement of a constriction ring. They are effective regardless of vascular impairment and are often recommended for men who cannot tolerate PDE5 inhibitors.
Second-line therapies
- Intracavernosal injections (e.g., alprostadil, combination therapies such as Trimix): Provide strong efficacy when oral medications fail.
- Intraurethral suppositories (alprostadil): Less commonly used but still available.
Surgical options
For men with severe, treatment-resistant ED, penile prosthesis implantation remains the most definitive solution. Satisfaction rates in diabetic men are high when performed by experienced surgeons, though infection risk is slightly elevated.
Future Directions: Innovations in 2025
Management of erectile dysfunction in men with diabetes continues to evolve. By 2025, several promising areas of research and new therapies are emerging:
Novel PDE5 inhibitor formulations
Researchers are developing sublingual and faster-acting forms of sildenafil and tadalafil, designed to improve onset time and minimize gastrointestinal side effects.
Combination therapies
Trials are exploring the combination of PDE5 inhibitors with antioxidants, statins, or L-arginine supplements to target multiple mechanisms simultaneously vascular inflammation, endothelial dysfunction, and nitric oxide deficiency. Early data suggest these combinations may improve outcomes in men with poorly controlled diabetes.
Regenerative medicine
Stem cell therapy and platelet-rich plasma (PRP) injections are being studied for their potential to regenerate damaged penile nerves and blood vessels. While still experimental, early-phase clinical trials report encouraging improvements in erectile rigidity in diabetic men.
Digital health and telemedicine
Telehealth platforms in 2025 now integrate glucose monitoring, cardiovascular tracking, and sexual health questionnaires. This allows endocrinologists and urologists to collaborate more efficiently, catching early signs of sexual dysfunction and adjusting treatment in real time.
Personalized medicine
Advances in genetic testing and biomarker analysis may soon allow physicians to predict which men with diabetes are more likely to develop ED, enabling earlier interventions.
Although these innovations are not yet mainstream, they highlight an important truth: erectile dysfunction in men with diabetes is no longer considered an inevitable outcome. With continuous research and comprehensive care, prognosis continues to improve.
Lifestyle Interventions
Lifestyle modification is the cornerstone of preserving sexual health in men with diabetes. Decades of research confirm that interventions targeting cardiovascular risk factors also improve erectile function.
- Dietary control and HbA1c optimization: Tight glycemic control reduces endothelial damage. Achieving an HbA1c < 7% is associated with a lower prevalence of ED.
- Exercise: Regular aerobic and resistance training improve vascular health, testosterone levels, and overall energy.
- Weight loss: Even a 5–10% reduction in body weight significantly improves erectile function scores.
- Smoking cessation: Smoking accelerates vascular damage. Quitting is among the most impactful lifestyle decisions for protecting potency.
Diabetes Management Strategies vs Effect on Sexual Function
| Strategy | Effect on Diabetes Control | Effect on Sexual Function |
| Diet and HbA1c control | Improves blood sugar, reduces complications | Preserves vascular health, lowers ED risk |
| Regular exercise | Improves insulin sensitivity, weight control | Enhances circulation, boosts testosterone |
| Weight loss | Reduces insulin resistance | Improves erectile function, libido |
| Smoking cessation | Lowers cardiovascular risk | Protects blood vessels, improves erection quality |
For more detail on the importance of lifestyle, see How lifestyle affects erectile function: sleep, diet, exercise, and stress.
Prevention: Regular Urology and Endocrinology Check-Ups
Prevention is central in protecting diabetes sexual health in men. Regular medical check-ups allow for early detection of risk factors and intervention before irreversible damage occurs.
- Urology visits: Men with diabetes should have routine urologic evaluations, particularly if they notice early signs of erectile difficulty. Urologists can recommend appropriate therapy and rule out other genitourinary conditions.
- Endocrinology visits: Endocrinologists ensure optimal glycemic control, screen for hypogonadism, and adjust therapies that may affect sexual function.
- Cardiology collaboration: Because ED is a predictor of cardiovascular events, men with diabetes and ED should also be assessed for underlying heart disease.
Ultimately, coordinated care between specialists offers the best chance of preserving potency. For men already affected, see Erectile dysfunction: how to regain strength and confidence.
Protecting Sexual Health in Men with Diabetes: 2025 Outlook
By 2025, the understanding of diabetes and men’s sexual health is deeper than ever. Vascular and neurological damage remain central mechanisms, but psychological factors and relationship stress also play a crucial role. Treatment options have expanded beyond PDE5 inhibitors to include hormone therapy, devices, and even emerging regenerative techniques. Lifestyle interventions diet, exercise, weight management, and smoking cessation remain powerful tools that improve both metabolic control and sexual function.
Most importantly, prevention through regular endocrinology and urology check-ups remains the key to protecting potency.Erectile dysfunction should not be accepted as an unavoidable consequence of diabetes. With early diagnosis, evidence-based therapy, and support, men can maintain both health and intimacy well into later life.
FAQ: Diabetes and Sexual Health in Men
Does every man with diabetes eventually develop erectile dysfunction?
No. While the risk is higher, good glycemic control, healthy lifestyle, and early treatment can significantly reduce the likelihood.
Why do PDE5 inhibitors sometimes work less effectively in men with diabetes?
Because diabetes causes both vascular and nerve damage, medications that rely on nitric oxide signaling may be less effective. In such cases, combination therapy or device-based solutions can help.
Can lifestyle changes alone reverse ED in diabetes?
In early stages, yes. Weight loss, exercise, and smoking cessation often lead to meaningful improvement. In advanced stages, lifestyle changes improve overall health but usually need to be combined with medical therapy.
Is testosterone therapy safe for men with diabetes?
When hypogonadism is confirmed, testosterone therapy can improve sexual desire and response to ED medication. However, it requires close monitoring by an endocrinologist or urologist.
Can ED be the first sign of diabetes?
Yes. Erectile dysfunction may appear years before diabetes is diagnosed, because vascular changes develop early. Men with new-onset ED should be screened for metabolic disease.
References
- American Diabetes Association – Sex and Diabetes
- Mayo Clinic – Erectile dysfunction and diabetes: Take control today
- Cleveland Clinic – The Link Between Diabetes and Sexual Dysfunction
- PubMed – The management of erectile dysfunction in men with diabetes mellitus who failed PDE5 inhibitors (2023)
- NIH (NIDDK) – Diabetes, Sexual, & Bladder Problems
