Antidepressants are among the most widely prescribed medicines in 2025, and for many men they are essential for staying well. At the same time, sexual function is a cornerstone of quality of life and treatment adherence. If libido drops, erections weaken, or orgasm becomes difficult after starting therapy, men often quietly reduce doses or stop altogether. The good news: most sexual side effects are predictable, explainable, and manageable without sacrificing mental health.
A practical way to think about this: antidepressants influence the same brain and peripheral pathways that regulate sexual desire, arousal, and climax. When therapy is effective for mood but problematic for sex, the goal isn’t to choose between mind and body – it’s to adjust the plan so both work well.
How antidepressants impact sexual function (SSRIs, SNRIs, TCAs)
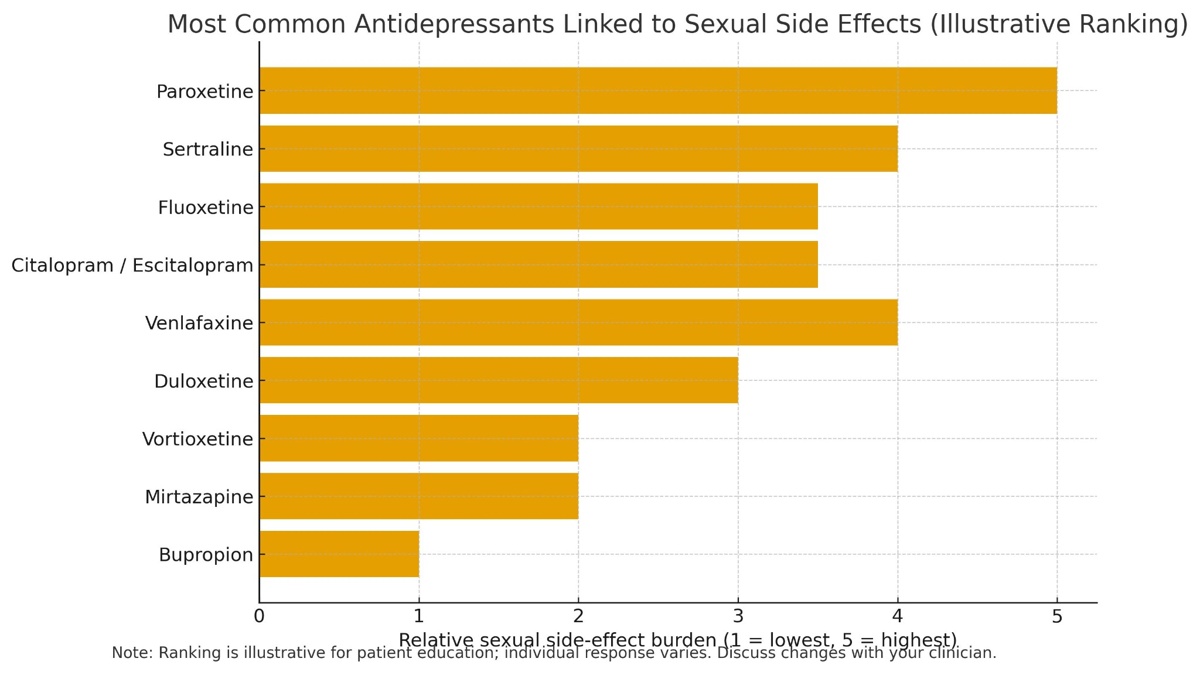
The effects differ by class and even by molecule. Selective serotonin reuptake inhibitors (SSRIs) increase synaptic serotonin to lift mood, but heightened serotonin tone can dampen dopaminergic drive and blunt nitric-oxide–mediated arousal. That’s why SSRIs are the class most often linked to reduced libido, erectile difficulties, and delayed ejaculation or orgasm. Among SSRIs, real-world experience consistently flags paroxetine as the most likely to cause sexual side effects, while sertraline and fluoxetine are common contributors as well. Some newer agents with mixed mechanisms (e.g., vortioxetine, vilazodone) are often perceived as easier on sexual function, though responses vary.
Serotonin–norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine and duloxetine may mirror SSRI-type effects because they still raise serotonin, even though norepinephrine can improve energy and attention for some users. Tricyclic antidepressants (TCAs) are older and pharmacologically “messier.” Clomipramine is notably associated with orgasmic delay; others (e.g., amitriptyline, nortriptyline) can impair function via anticholinergic sedation or secondary serotonin reuptake effects.
Two important counterpoints help men avoid over-generalizing. First, depression itself can lower libido and cause erectile problems; sometimes improvement in mood improves sex, even on the same medicine. Second, individual variability is large: dose, metabolism, comorbidities (sleep apnea, diabetes, low testosterone), and other medicines (finasteride, some antihypertensives) all shape outcomes. That’s why smart management focuses on tailored adjustments rather than one-size-fits-all rules.
Most Common Antidepressants Linked to Sexual Side Effects
Symptoms: decreased libido, erectile dysfunction, delayed orgasm
Sexual side effects usually cluster in three domains, and men may experience one, two, or all three:
- Decreased libido (desire): Feels like “the mind isn’t interested.” Often appears first after dose increases.
- Erectile dysfunction (arousal): Difficulty achieving or maintaining a firm erection; morning/nocturnal erections may lessen.
- Delayed orgasm/ejaculation (climax): Time to climax stretches or orgasm becomes unattainable; some men describe reduced genital sensitivity.
A few practical signals help distinguish medication effects from the depression itself. If mood has clearly improved but sexual function has worsened in parallel with starting or raising the dose, medication is a likely driver.If libido and energy were low before treatment and improved alongside mood, the condition not the drug may have been primary.
Managing side effects (dose adjustment, drug switching, add-on therapies)
The goal in 2025 is to keep depression in remission and protect sexual health. When men report antidepressants erectile dysfunction or other SSRI sexual side effects, clinicians typically follow a stepwise, reversible strategy that minimizes relapse risk while restoring desire, erections, and orgasm.
A practical playbook that works in real clinics
- Reassess the dose and timing. Many SSRI sexual side effects are dose-dependent. If mood is stable, a modest dose reduction (while monitoring symptoms) can improve libido and erection quality without destabilizing mood. Adjusting dose timing (e.g., evening dosing for sedating agents) sometimes lessens perceived sexual blunting.
- Switch to a sex-friendlier antidepressant. If side effects persist, consider moving from a high-burden SSRI (e.g., paroxetine) to options with better sexual tolerability, such as bupropion or, in some cases, vortioxetine or mirtazapine. This approach targets the root cause rather than “layering” fixes.
- Add-on therapies targeted to the specific problem. When switching isn’t feasible, adjuncts can salvage sexual function:
- For erectile function: on-demand PDE5 inhibitors (e.g., sildenafil, tadalafil) are effective for antidepressants erectile dysfunction, provided there are no nitrate interactions.
- For low libido: adding bupropion (dopamine/norepinephrine effects) can offset serotonergic sexual blunting.
- For delayed orgasm: small dose reductions or switching off the most serotonergic agents often help; occasionally, carefully chosen adjuncts (e.g., buspirone) are considered case-by-case.
- Address contributing medical factors. Sleep apnea, obesity, diabetes, hypertension, low testosterone, and relationship stress frequently amplify depression and ED. Treating these raises the ceiling for sexual recovery.
- Avoid “drug holidays.” Skipping SSRI doses around anticipated sex risks relapse and withdrawal symptoms; it’s not a 2025-standard strategy.
Throughout, the message to patients is simple: sexual side effects are manageable; don’t abandon treatment – optimize it.
Antidepressants vs sexual side effects (severity & notes)
| Antidepressant | Relative sexual side-effect burden* | Typical sexual effects | Notes for 2025 management |
|---|---|---|---|
| Paroxetine | High | Marked libido reduction, delayed orgasm, antidepressants erectile dysfunction | Often first to switch away from if SSRI sexual side effects dominate |
| Sertraline | Moderate–High | Decreased desire, delayed ejaculation/orgasm | Consider dose reduction or switch if persistent |
| Fluoxetine | Moderate | Reduced libido, delayed orgasm | Long half-life; changes take longer to equilibrate |
| Bupropion | Low (often pro-sexual) | May improve desire/arousal | Useful as switch or add-on in depression and ED |
Relative burden is a clinical generalization; individual response varies.
Role of dapoxetine in premature ejaculation
Dapoxetine is an on-demand SSRI designed specifically for premature ejaculation (PE). Unlike standard SSRIs used daily for mood, dapoxetine is taken before sexual activity and is not intended to treat depression. For men whose core complaint is rapid ejaculation rather than antidepressants erectile dysfunction, dapoxetine can significantly extend intravaginal latency time and improve control and satisfaction. Because it is short-acting, it has a more favorable day-to-day side-effect profile than chronic SSRIs, and it can be integrated with PDE5 inhibitors when PE coexists with ED under medical supervision.
For readers exploring PE-focused therapy, see our detailed guide to dapoxetine (Priligy) placed within the PE section of the site it explains dosing windows, who benefits most, and safety considerations . If anxiety or performance stress is a major driver, pairing PE treatment with psychological support often yields better and more durable results; we expand on mind-body links in our upcoming piece on Psychological Erectile Dysfunction (Article #7, internal link to be placed when live)
When to seek combined psychiatric and urologic care
Sometimes SSRI sexual side effects persist despite sensible first steps (dose review, timing changes, or a switch). And sometimes depression and ED amplify each other: low mood undermines desire and function, while sexual problems undermine adherence and mood. In those cases, the most efficient route is coordinated care between mental-health and sexual-medicine clinicians.
A brief roadmap that’s patient-friendly and realistic in 2025:
- Bring in both specialists if you have ongoing antidepressants erectile dysfunction, marked loss of desire, or persistent orgasmic delay after an initial medication adjustment.
- Let psychiatry protect remission (confirm stability, consider a dose tweak or switch to a sex-friendlier agent like bupropion, vortioxetine, or mirtazapine where appropriate).
- Let urology personalize sexual recovery (screen cardiovascular risks, diabetes, sleep apnea, and low testosterone; consider targeted add-ons such as PDE5 inhibitors for erections or on-demand dapoxetine for PE).
- Optimize foundations sleep quality, exercise, weight, alcohol, and relationship dynamics because these levers meaningfully shift outcomes for depression and ED.
This two-pronged approach keeps the antidepressant plan effective and restores satisfying sexual function. It also reduces the temptation to self-adjust or stop medication, which is a major reason for relapse.
Persistent fatigue, low energy, and non-restorative sleep often travel with low libido and antidepressants erectile dysfunction; for a deeper dive into work-up and fixes, explore Chronic Fatigue and Sexual Function
FAQ: Antidepressants and Sexual Function (2025)
Can I have ED and still get nocturnal or morning erections?
Yes. With psychogenic components, men may have normal night/morning erections yet face performance-related ED. With organic factors (vascular, hormonal, neurologic), erections often weaken both day and night. Managing depression and ED together is key.
Which antidepressants are most associated with sexual side effects?
Among SSRIs, paroxetine is frequently reported as highest burden; sertraline and fluoxetine are common contributors. SNRIs can show similar patterns. Some agents (e.g., bupropion) tend to be more favorable for sexual function. Individual response varies.
What are the hallmark symptoms?
Reduced libido, antidepressants erectile dysfunction (trouble achieving/maintaining rigidity), and delayed or absent orgasm/ejaculation. Any of these can appear alone or together.
What’s the first management step?
Don’t stop the medicine on your own. Discuss a dose adjustment or timing change; if inadequate, consider switching to a better-tolerated agent or using add-on therapies (e.g., PDE5 inhibitors, bupropion).
Is “drug holiday” a good idea for sex?
Not recommended. Irregular dosing risks relapse, discontinuation symptoms, and inconsistent sexual effects.
Where does dapoxetine fit?
It’s for premature ejaculation, taken on demand, and can coexist with a stable antidepressant plan. It does not treat mood.
When should I see both a psychiatrist and a urologist?
When problems persist after basic adjustments, when SSRI sexual side effects drive nonadherence, or when ED presents alongside cardiometabolic risks, low testosterone, or sleep issues.
References (verified, working links)
- Mayo Clinic – Antidepressants: Which cause the fewest sexual side effects?
- PubMed – Management of Antidepressant-Induced Sexual Dysfunction: A Literature Review (Cureus, 2025)
- PubMed – Antidepressant-induced sexual dysfunction (overview)
- Cleveland Clinic – SSRIs: Uses, Types & Side Effects (sexual dysfunction noted)
- NIH / NCBI Bookshelf – Antidepressants (StatPearls)
