In recent years, testosterone replacement therapy (TRT) has become a common and effective treatment for male hypogonadism and gender-affirming hormone therapy in the United States. With an increasing number of patients transitioning from in-clinic administration to home testosterone injections, correct injection technique and patient education have become essential components of safe and effective therapy.
Improper technique can lead to preventable complications such as pain, local infection, oil infiltration, or—rarely—pulmonary oil microembolism (POME). Conversely, proper instruction in asepsis, needle selection, and injection speed significantly reduces adverse effects and improves treatment adherence.
This practical guide reviews how to inject testosterone safely, how to choose the right injection site and needle, how to store and dispose of testosterone vials, and how to recognize and manage potential complications. It is based on up-to-date recommendations from the American Urological Association (AUA) and current clinical guidelines as of 2025.
Choosing the Injection Site, Needle, and Volume
Understanding Injection Types: Intramuscular vs Subcutaneous
Testosterone can be administered by two primary methods:
- Intramuscular (IM) injections — typically using testosterone cypionate or enanthate in an oil-based carrier.
- Subcutaneous (SC) injections — increasingly used for lower doses or patients preferring smaller needles and less injection pain.
Both routes can provide stable testosterone levels when performed correctly, but intramuscular injections remain the standard for most long-acting formulations.
Guide to testosterone esters and how urologists select dosing schedules
Selecting the Injection Site: Deltoid, Thigh, or Gluteal Muscle
The injection site determines both absorption efficiency and risk of complications. The three most common intramuscular sites are:
| Site | Muscle | Recommended Needle | Volume Range | Advantages / Notes |
|---|---|---|---|---|
| Deltoid | Upper arm (lateral deltoid) | 22–23G, 1 inch | ≤ 1 mL | Convenient, but limited volume; suitable for smaller doses or SC route. |
| Thigh | Vastus lateralis (outer thigh) | 22–23G, 1–1.25 inch | 1–2 mL | Easy self-access, stable muscle mass; rotate sites weekly. |
| Gluteal | Ventrogluteal or dorsogluteal area | 21–22G, 1.5 inch | up to 3 mL | Preferred for large oil-based doses; deep IM reduces leakage. |
Pro tip: The ventrogluteal site is often safest, with fewer major blood vessels and nerves compared to the traditional dorsogluteal area.
Before every injection, visually inspect the site for redness, bruising, or lumps, and rotate sites with each dose to prevent lipodystrophy or infiltrates.
Choosing the Right Needle Gauge and Length
Selecting the correct needle ensures proper drug delivery and minimizes tissue trauma.
Gauge: For drawing thick oil-based testosterone (e.g., cypionate or enanthate), a 18–20G needle can be used to load the syringe. Then, switch to a 22–23G needle for actual injection to reduce discomfort.
Length: Use 1–1.5 inch for intramuscular delivery (gluteal or thigh), and ½ inch for subcutaneous injections.
Angle: IM injections should be inserted at a 90-degree angle; SC at 45 degrees.
Inject slowly—approximately 1 mL over 10 seconds—to minimize pressure and pain. Rapid injection increases the chance of infiltration or leakage of the oil-based solution.
Managing Oil-Based Testosterone Formulations
Most testosterone replacement products in the U.S. (e.g., Testosterone Cypionate, Enanthate, and Undecanoate) are suspended in sesame or cottonseed oil. These solutions are viscous, meaning they require more time to draw and inject.
- Warm the vial slightly (by holding it in your hand for 1–2 minutes) to reduce viscosity.
- Draw the exact prescribed dose and check for air bubbles before injection.
- Never mix testosterone with other medications in the same syringe.
- Aspirate gently before injecting to ensure the needle is not in a blood vessel.
- Although rare, pulmonary oil microembolism (POME) can occur if oil enters the bloodstream. Symptoms such as cough, chest tightness, or dizziness shortly after injection require immediate medical attention.
Key Takeaway
Choosing the correct site, using the proper needle gauge, and injecting slowly are fundamental to preventing complications and ensuring optimal absorption of testosterone. For patients performing home testosterone injections, these details make the difference between a safe, comfortable experience and one that results in unnecessary pain or adverse reactions.
Asepsis, Storage, and Disposal
Aseptic Technique
Maintaining sterility during testosterone injections is essential to prevent infection and ensure consistent absorption of the medication. Even minor contamination of an oil-based testosterone solution can result in cellulitis, abscess formation, or systemic infection. The same clinical hygiene standards applied in a medical office must also be followed during home injections.
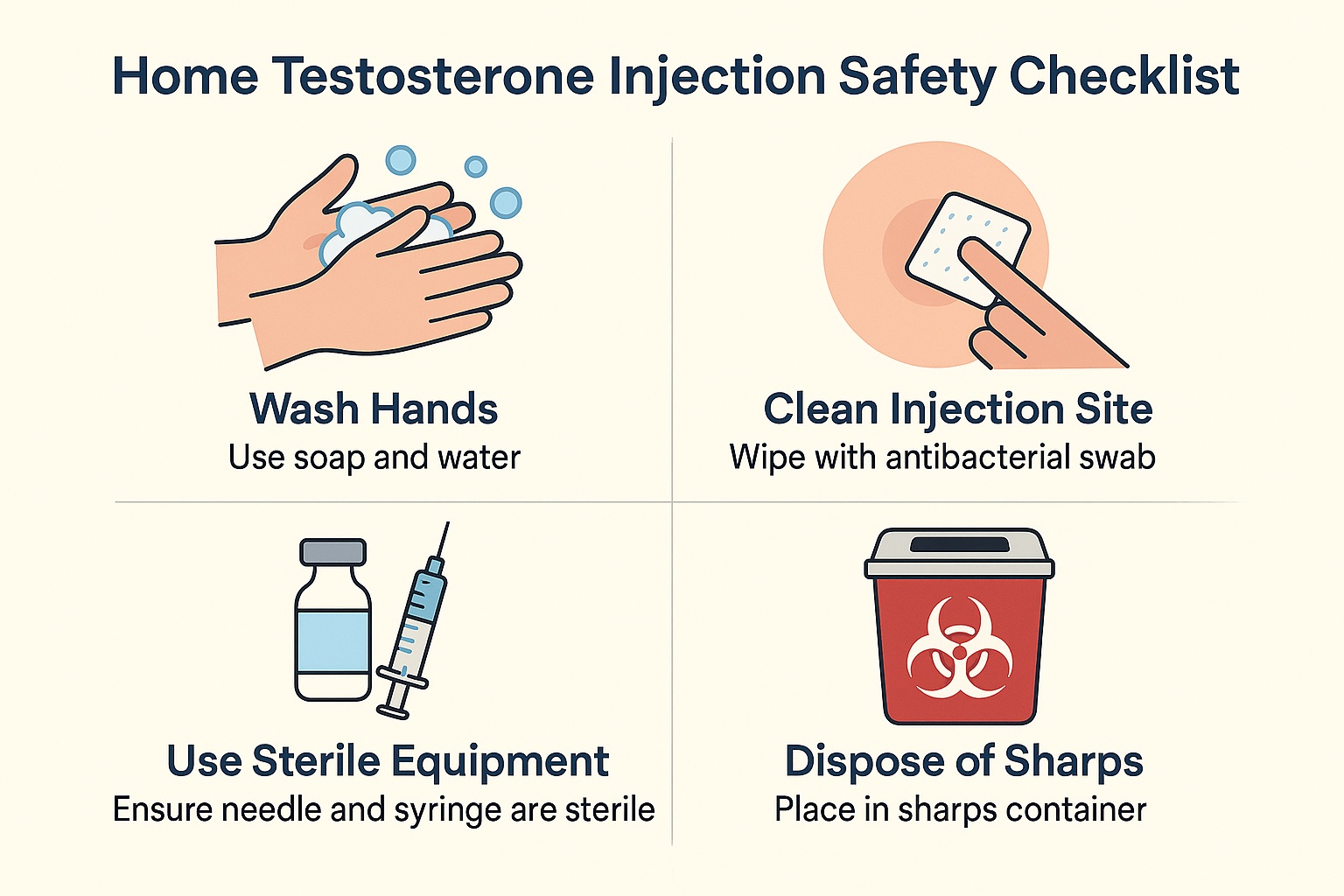
Aseptic technique begins with proper preparation. The patient should wash their hands thoroughly with soap and warm water for at least twenty seconds and prepare a clean, well-lit workspace. All injection materials vial, syringe, needles, alcohol swabs, and a sterile cotton ball should be arranged on a disinfected surface.
Before each injection, the rubber stopper on the testosterone vial must be disinfected with a 70% isopropyl alcohol wipe and allowed to dry completely. A new, sterile syringe and two separate needles are required: one for drawing up the medication and another for injection. The drawing needle should never be used to inject, as it becomes dulled during vial penetration and increases tissue trauma.
Once the correct dose is drawn, the needle should not touch any unsterile surface. The injection site (deltoid, thigh, or gluteal muscle) must also be cleaned with alcohol and allowed to air dry before injection. Injecting through wet alcohol can increase stinging and does not improve disinfection.
Proper asepsis also extends to personal behavior. Talking or breathing directly over open equipment should be avoided, and reusable materials must not be used. Hands should remain below shoulder level and above the clean field during the procedure.
Storage of Testosterone Vials
Appropriate storage ensures the stability and potency of testosterone preparations. Oil-based esters such as testosterone cypionate or enanthate are generally stable when stored at controlled room temperature between 68 and 77 °F (20–25 °C). They should be kept away from direct sunlight, moisture, and excessive heat.
The vials must be stored upright and tightly sealed to prevent leakage or contamination. Refrigeration is not recommended unless specifically instructed by the manufacturer, as cooling increases oil viscosity and may cause crystallization of the active substance.
After the vial is opened, it should be dated and used within 28 days, unless otherwise specified in the package insert. Before each use, the solution must be inspected for clarity and absence of particulates. A cloudy or discolored solution indicates degradation or contamination and should be discarded.
The following table summarizes proper storage conditions:
| Condition | Recommendation | Purpose |
|---|---|---|
| Temperature | 68–77 °F (20–25 °C) | Maintains chemical stability |
| Light exposure | Store in a dark cabinet | Prevents oxidation |
| Position | Upright, tightly sealed | Prevents leakage |
| Refrigeration | Not required | Avoids crystallization |
| After opening | Use within 28 days | Reduces contamination risk |
Failure to maintain correct storage conditions can alter the pharmacokinetics of testosterone, leading to unpredictable serum levels or loss of efficacy.
Disposal of Sharps and Used Materials
Safe disposal of syringes, needles, and vials is a critical component of home testosterone therapy. Improper disposal increases the risk of accidental needle-stick injuries and potential transmission of bloodborne pathogens.
Used needles and syringes must be placed immediately into a puncture-resistant, FDA-approved sharps container without recapping. The container should be kept out of reach of children and pets. When the container is three-quarters full, it must be sealed and taken to a designated collection site, such as a pharmacy, hospital, or community hazardous waste program.
Used vials should be disposed of according to local or state regulations. Many U.S. states prohibit disposal of medical sharps and drug containers in regular household trash.
Alcohol pads, gauze, and packaging that are not contaminated with blood may be discarded in regular household waste.
The table below summarizes disposal procedures:
| Item | Disposal Method | Rationale |
|---|---|---|
| Needle and syringe | Place in an approved sharps container | Prevents needle-stick injuries |
| Used vial | Return to pharmacy or hazardous waste facility | Avoids environmental contamination |
| Alcohol pads and gauze | Dispose in household trash | Low infection risk |
Adherence to aseptic technique, proper storage, and responsible disposal practices forms the foundation of safe testosterone therapy. Each injection must be treated as a sterile procedure, whether performed by a healthcare provider or at home. Maintaining sterility protects the patient from infection, ensures drug potency, and supports long-term treatment adherence. Patients who receive structured education in these procedures consistently report fewer injection-site complications and higher satisfaction with therapy outcomes.
Home Administration, Monitoring, and Follow-Up
Clinic-based injections ensure professional oversight and immediate response to complications, making them ideal for new or high-risk patients.
Home administration, once a patient demonstrates proper aseptic technique and injection accuracy, increases independence and treatment adherence.
Comparison of Home vs Clinic Administration
| Factor | Home Injection | Nurse Administration |
|---|---|---|
| Accessibility | Flexible scheduling and privacy | Requires in-person appointment |
| Oversight | Self-monitored with scheduled reviews | Continuous professional supervision |
| Cost | Lower long-term expense | Higher per-visit cost |
| Training | Patient education required | Performed by medical staff |
| Recommended for | Stable, competent adults | New or high-risk individuals |
Training and Technique Verification
Before approving self-administration, clinicians must verify the patient’s competence through direct observation or telehealth demonstration.
Retraining and technique review should occur every six to twelve months to maintain safety standards.
Patients should keep a detailed injection log noting the site, dose, and any reactions or pain levels.
Missed Dose Protocol
If the injection is missed by a few days, administer it as soon as possible and continue the regular schedule.
If more than two weeks have passed, or the patient is unsure when the last dose was given, contact the prescriber before injecting.
Never double the next dose, as this may cause supraphysiologic testosterone levels and adverse effects.
When to Contact a Physician
- Seek medical evaluation if pain, redness, or swelling at the injection site persists longer than 48 hours.
- Fever, cough, or chest discomfort immediately after injection may indicate pulmonary oil microembolism and require urgent care.
- Regular follow-up every three to six months should include testosterone level checks, hematocrit, lipid profile, and PSA for adult men.
FAQ – Frequently Asked Questions
Can I inject into the same muscle every time?
No. Rotating sites prevents scar tissue, inflammation, and irregular absorption, which can alter hormone levels over time. Use opposite sides of the body for each new injection.
Why does oil-based testosterone sometimes cause pain?
Oil formulations move slowly through tissue, creating pressure and soreness. Injecting slowly and relaxing the muscle can reduce pain, and warming the vial beforehand lowers viscosity.
What should I do if some medication leaks out after injection?
Minor leakage is common and usually harmless. Applying light pressure with sterile gauze for 30 seconds prevents further loss and promotes absorption.
Is subcutaneous injection an acceptable alternative to intramuscular administration?
Yes, in selected cases. Subcutaneous injections can offer more stable hormone levels and less post-injection pain, but they must be specifically approved by the treating clinician.
How long can an opened vial be used safely?
Most multi-dose testosterone vials remain safe for 28 days after first puncture. After this period, bacterial contamination risk increases, and the vial should be discarded even if not empty.
What if I accidentally inject into a blood vessel?
Stop immediately if blood appears in the syringe during aspiration. Replace the needle and inject at a different site after confirming no blood return before injection.
Can I travel with testosterone?
Yes. Keep vials in original labeled packaging at room temperature and carry a copy of the prescription or a doctor’s letter for airport security checks.
