Testosterone replacement therapy (TRT) continues to grow in popularity across the United States, driven by greater awareness of male hypogonadism and the availability of effective injectable formulations. Yet as use expands, so do questions about long-term safety. Concerns often center on three systems: the blood, the prostate, and the heart.
The latest evidence, including the TRAVERSE Trial published in the New England Journal of Medicine (2023) and the 2025 updates from the Endocrine Society and American Urological Association, provides reassuring clarity. When testosterone injections are prescribed for properly diagnosed hypogonadism and monitored according to modern standards, they are safe for most men.
When testosterone therapy is truly indicated in clinical practice
Still, safety depends on vigilance. Testosterone influences hematopoiesis, lipid metabolism, and prostate growth. Regular laboratory testing hematocrit, PSA, estradiol, and lipid panels remains central to minimizing risk. The goal of monitoring is not to limit therapy but to ensure that its physiological benefits do not drift into supraphysiologic territory.
The following sections outline what to watch, how often to measure, and how to interpret the results within the 2025 clinical context.
Erythrocytosis and Hematocrit: Thresholds and Correction
Physiological background
Among all laboratory changes seen during testosterone therapy, erythrocytosis is the most predictable. Testosterone stimulates erythropoietin production in the kidneys, which in turn increases red blood cell synthesis in the bone marrow. Moderate elevation of hematocrit is part of the intended anabolic effect it improves oxygen delivery and muscle performance. The problem begins when the hematocrit exceeds safe limits, thickening the blood and predisposing to vascular events.
Risk profile of injectable formulations
Injectable esters such as testosterone cypionate or enanthate create high serum peaks shortly after administration. These transient surges strongly stimulate erythropoiesis, explaining why erythrocytosis is reported in up to 15–20 percent of men using weekly injections, compared with fewer than 5 percent on transdermal therapy. Long-acting undecanoate formulations produce steadier levels and a lower incidence of elevated hematocrit.
Differences between testosterone esters and how to choose the right dosing schedule
Thresholds and monitoring intervals
Current U.S. guidelines define the safe hematocrit range as below 52 percent. Values between 50 and 52 percent require closer observation; those above 52 percent call for dose adjustment or temporary suspension of therapy. Persistent levels exceeding 54 percent may warrant therapeutic phlebotomy.
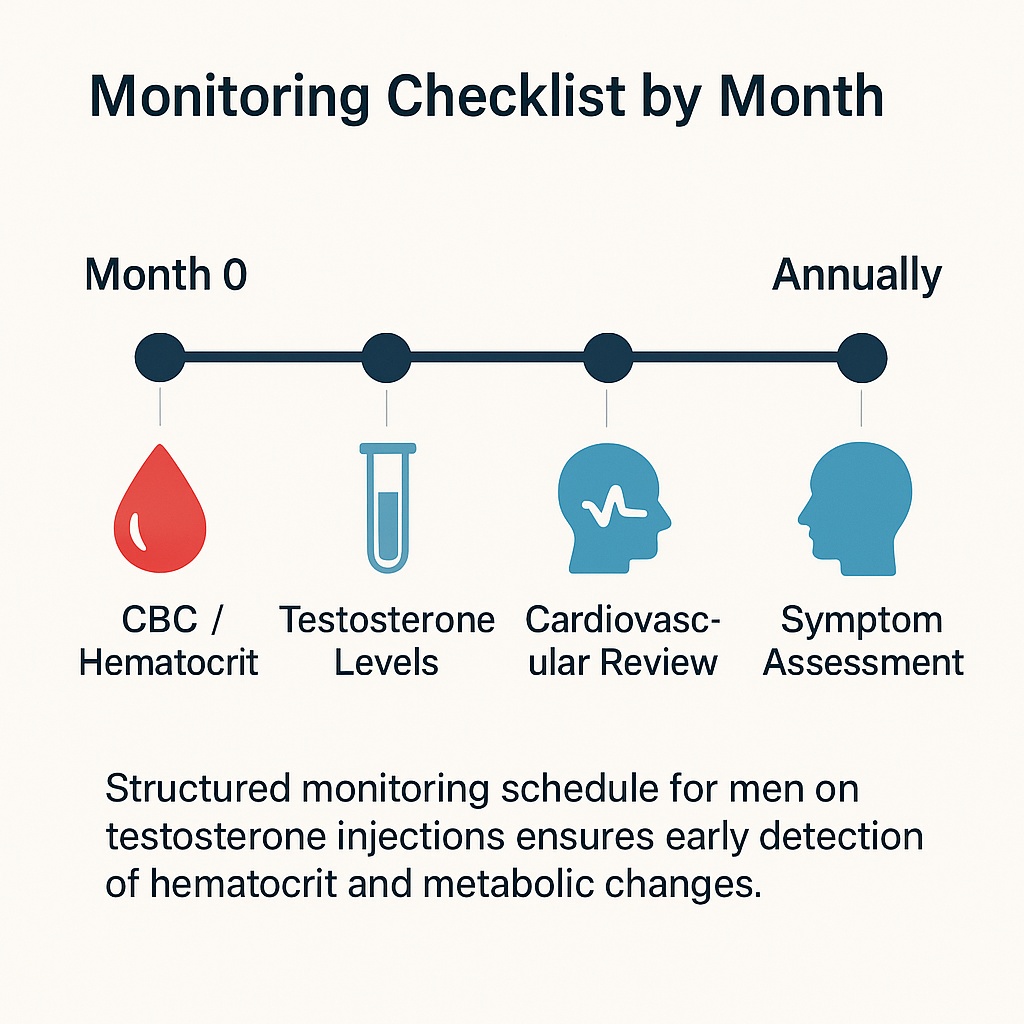
Monitoring should follow a fixed schedule:
- Baseline measurement before the first injection,
- Re-evaluation at three months, six months, and twelve months,
- Annual testing thereafter if values remain stable.
Men living at high altitude, smokers, or patients with chronic pulmonary disease may require more frequent checks.
Management strategy
When hematocrit approaches the threshold, physicians usually lower the testosterone dose or lengthen the injection interval. If elevation persists, switching to a transdermal or long-acting injectable formulation can help stabilize serum levels. For hematocrit above 54 percent, phlebotomy effectively and rapidly reduces viscosity. Contributing factors such as dehydration or untreated sleep apnea should always be corrected concurrently.
Therapy should only be paused when hematocrit remains uncontrolled despite these adjustments or when the patient develops symptoms consistent with hyperviscosity: facial redness, headaches, blurred vision, or shortness of breath. After normalization, treatment may resume at a reduced dose.
Patient counseling and clinical insight
Men often perceive higher testosterone levels as inherently better. Clinicians must emphasize that normalization, not maximization, ensures safety. Most benefits improved energy, libido, and cognition occur when serum testosterone remains in the mid-physiologic range (400–700 ng/dL). Exceeding that window increases the likelihood of erythrocytosis without additional clinical gain.
Educating patients to recognize early warning signs and to maintain adequate hydration is part of modern TRT practice. A brief discussion at each follow-up visit often prevents complications later.
Target Laboratory Ranges and Actions (2025)
| Parameter | Target Range | Action Threshold | Recommended Action |
|---|---|---|---|
| Hematocrit | 42–50 % | > 52 % | Reduce dose / extend interval |
| Hemoglobin | 13–17 g/dL | > 18 g/dL | Re-evaluate formulation |
| Red Cell Count | Within normal limits | Rising trend | Assess OSA / hydration status |
Cardiovascular Risk and Testosterone Therapy: 2025 Evidence and Clinical Guidance
Cardiovascular safety has long been the most debated aspect of testosterone therapy.Early observational studies raised alarms about increased myocardial infarction risk, yet these findings were limited by poor patient selection and confounding factors such as obesity, smoking, and untreated sleep apnea.
Latest evidence and regulatory update
The landmark TRAVERSE Trial (NEJM, 2023), a multicenter, randomized controlled study involving more than 5,000 men, finally addressed the controversy. It found no significant increase in major adverse cardiovascular events (MACE) among men treated with testosterone compared with placebo. Based on these findings, the FDA updated its labeling in 2024, removing the prior “heart attack” warning and emphasizing physician-led risk assessment instead.
Who remains at higher risk
Despite the overall safety signal, not all men have the same cardiovascular resilience. Special caution applies to those with:
- Recent myocardial infarction or stroke (within six months)
- Uncontrolled congestive heart failure
- Severe untreated obstructive sleep apnea (OSA)
- Uncontrolled hypertension
For these men, testosterone may still be used once their condition stabilizes and only under joint supervision of endocrinology and cardiology specialists.
Monitoring cardiovascular parameters
Modern testosterone replacement therapy monitoring protocols focus on overall metabolic health rather than testosterone alone. At baseline and during follow-up visits, physicians measure blood pressure, lipid profile, fasting glucose or HbA1c, and body composition. Repeat evaluation every six to twelve months ensures that therapy does not mask or exacerbate underlying disease.
Men on TRT often experience favorable metabolic changes reduction in fat mass, modest increase in HDL cholesterol, and improved insulin sensitivity especially when therapy is combined with exercise and diet optimization.
Practical clinical approach
Testosterone therapy should not be initiated in men with acute coronary syndromes, nor should it replace standard management of hypertension, diabetes, or dyslipidemia. Instead, TRT works best as part of an integrated health plan. Encouraging smoking cessation, weight control, and consistent physical activity maximizes benefits while reducing any theoretical risks.
In 2025, most experts view testosterone therapy as cardiometabolically neutral or beneficial when prescribed responsibly. The therapy is not a panacea but also not a threat when evidence-based protocols are followed.

Managing Estradiol, Edema, Sleep Apnea, Acne, and Gynecomastia During Testosterone Therapy
Testosterone therapy is rarely a single-axis intervention. As serum testosterone rises, a portion converts into estradiol (E2) through the aromatase enzyme, particularly in men with higher body fat. While estradiol is essential for libido, bone density, and cardiovascular function, excessive levels may produce unwanted effects such as fluid retention, acne, mood swings, or gynecomastia.
Understanding estradiol balance
The optimal estradiol range for men on testosterone therapy typically falls between 20 and 40 pg/mL. Below this level, men may experience joint stiffness, fatigue, or low mood; above it, water retention and breast tenderness become more likely. Monitoring estradiol is therefore an individualized decision. In most men, testing is reserved for those who develop symptoms rather than performed routinely.
Clinical management strategies
When estrogen-related side effects occur, physicians focus first on dose adjustment lowering the testosterone amount or extending the injection interval. This approach often normalizes estradiol without additional medication. If symptoms persist, aromatase inhibitors such as anastrozole may be introduced at low, intermittent doses under strict supervision. The goal is to restore balance, not to eliminate estradiol completely, as too little carries its own metabolic risks.
Edema, or ankle swelling, appears in the early weeks of therapy as the body rebalances fluid distribution. Adequate hydration, dietary sodium control, and slower titration of testosterone reduce this effect. Persistent swelling or shortness of breath should prompt cardiovascular evaluation.
Sleep apnea can also intensify during TRT, particularly in obese men or those with pre-existing apnea. Continuous positive airway pressure (CPAP) remains the gold standard treatment. Addressing apnea not only improves sleep quality but also reduces the likelihood of erythrocytosis and morning headaches.
Acne results from androgenic stimulation of sebaceous glands. Topical benzoyl peroxide or retinoid therapy is usually effective. For resistant cases, dermatologic consultation is recommended rather than discontinuing testosterone.
Gynecomastia enlargement of male breast tissue occurs when estradiol levels remain elevated for prolonged periods. Early recognition allows non-invasive management: dose adjustment and short-term aromatase inhibition. Chronic cases with fibrotic changes may require surgical correction, though such outcomes are rare with modern dosing protocols.
In 2025, endocrinologists emphasize symptom-guided monitoring. Laboratory numbers are valuable, but patient experience — energy levels, mood, body composition, and sleep quality defines true therapeutic success.
Laboratory Protocol and Target Monitoring Ranges (2025 Edition)
Effective monitoring transforms testosterone therapy from an art into a precise, data-driven practice. Current guidelines from the Endocrine Society, AUA, and the VA Formulary 2025 outline a standardized protocol for both initiation and maintenance phases.
At baseline, clinicians record total and free testosterone, hematocrit, PSA, lipid profile, glucose, and blood pressure. Estradiol and liver enzymes are optional but recommended for high-risk patients.
Follow-up occurs at three to six months, then annually once stability is achieved. Measurements should be taken at consistent times ideally in the morning and, for injectables, midway between doses to minimize variability.
Recommended Laboratory Monitoring Schedule (2025)
| Test | Baseline | 3–6 Months | 12 Months | Annual | Target Range / Notes |
|---|---|---|---|---|---|
| Total Testosterone (TT) | ✔️ | ✔️ | ✔️ | ✔️ | 400–700 ng/dL (mid-normal) |
| Free Testosterone (FT) | ✔️ | Optional | Optional | Optional | For men with abnormal SHBG |
| Estradiol (E2) | Optional | If symptomatic | As needed | As needed | 20–40 pg/mL |
| Hematocrit (Hct) | ✔️ | ✔️ | ✔️ | ✔️ | Maintain < 52 % |
| PSA | ✔️ | ✔️ | ✔️ | ✔️ | No increase > 1.4 ng/mL / yr |
| Lipid Panel / Glucose | ✔️ | Optional | ✔️ | ✔️ | For metabolic tracking |
Frequently Asked Questions (FAQ)
Is testosterone injection safe for long-term use?
Yes. Current data, including the 2023–2025 TRAVERSE follow-up, confirm that properly monitored TRT is safe for most men, provided hematocrit and cardiovascular parameters remain within target ranges.
How often should I have labs checked?
At baseline, 3–6 months, and annually once stable. More frequent testing may be required for men with heart disease or sleep apnea.
Do I need to test estradiol regularly?
Not unless symptoms suggest imbalance such as swelling, mood swings, or breast tenderness.
Can testosterone therapy cause prostate cancer?
No causal link has been demonstrated. Monitoring PSA ensures early detection of unrelated disease, not prevention of TRT-induced cancer.
What should I do if my hematocrit is high?
Work with your physician to reduce dose or extend injection intervals; if Hct > 54 %, temporary cessation or phlebotomy is recommended.
References
- Endocrine Society – Testosterone Therapy in Men With Hypogonadism: Clinical Practice Guideline
- American Urological Association (AUA) – Testosterone Deficiency Guideline
- U.S. Department of Veterans Affairs – Testosterone Replacement Therapy Criteria for Use (March 2025)
- New England Journal of Medicine – Cardiovascular Safety of Testosterone-Replacement Therapy (TRAVERSE Trial, 2023)
- PMC Open Access – Long Term Cardiovascular Safety of Testosterone Therapy
