Erectile health is not just a matter of intimacy; it is one of the clearest reflections of a man’s cardiovascular, hormonal, and neurological condition. Among the most reliable natural markers of this connection are nocturnal erections, medically referred to as nocturnal penile tumescence (NPT). These sleep-related erections, often unnoticed, play a much bigger role in men’s health than many realize.
Doctors have long used nocturnal erections to differentiate between organic causes of erectile dysfunction (ED) and psychological ones. By 2025, with more advanced home-monitoring technologies and growing awareness about male health, NPT has become a crucial tool in early detection of underlying diseases. Understanding what nocturnal erections are, why they happen, and what their absence may mean helps men move beyond the common myths about ED and approach their health from an informed perspective.
What are nocturnal penile tumescence (NPT) erections?
Nocturnal penile tumescence refers to spontaneous erections that take place while a man is asleep. A healthy male typically experiences between three and five erections during the night, each lasting up to an hour. They occur independently of sexual thoughts or stimulation and are instead linked to natural processes that maintain the health of penile tissue.
These erections usually happen during the REM stage of sleep, when brain activity increases and the body undergoes vivid dreaming. Their function is more mechanical than erotic: they help keep blood vessels and erectile tissue well-oxygenated and prevent long-term damage to the structure of the penis. Because they are involuntary, their presence or absence gives physicians valuable insight into whether erectile problems are rooted in physical dysfunction or psychological stress. That is why in modern clinical management of ED, NPT is still considered one of the most reliable diagnostic tools more about how urologists use this in daily practice.
Why do nocturnal erections occur during sleep?
Although the full biological explanation is still being studied, scientists have identified several mechanisms that make nocturnal erections a predictable event. During REM sleep, the parasympathetic nervous system becomes dominant, relaxing the smooth muscle in the penis and allowing blood to flow more easily. At the same time, testosterone levels peak in the early morning hours, which further supports erectile activity.
Another important role of these erections is maintaining oxygen supply to the penis. Without regular nocturnal erections, tissues could gradually lose elasticity, leading to fibrosis and impaired function. This automatic “maintenance cycle” keeps the penis healthy even in the absence of regular sexual activity.
There is also a neurological element: nocturnal erections act as a spinal reflex, triggered independently of erotic stimuli. In other words, they are part of the body’s natural rhythm, as reliable as the heartbeat or breathing patterns during sleep.
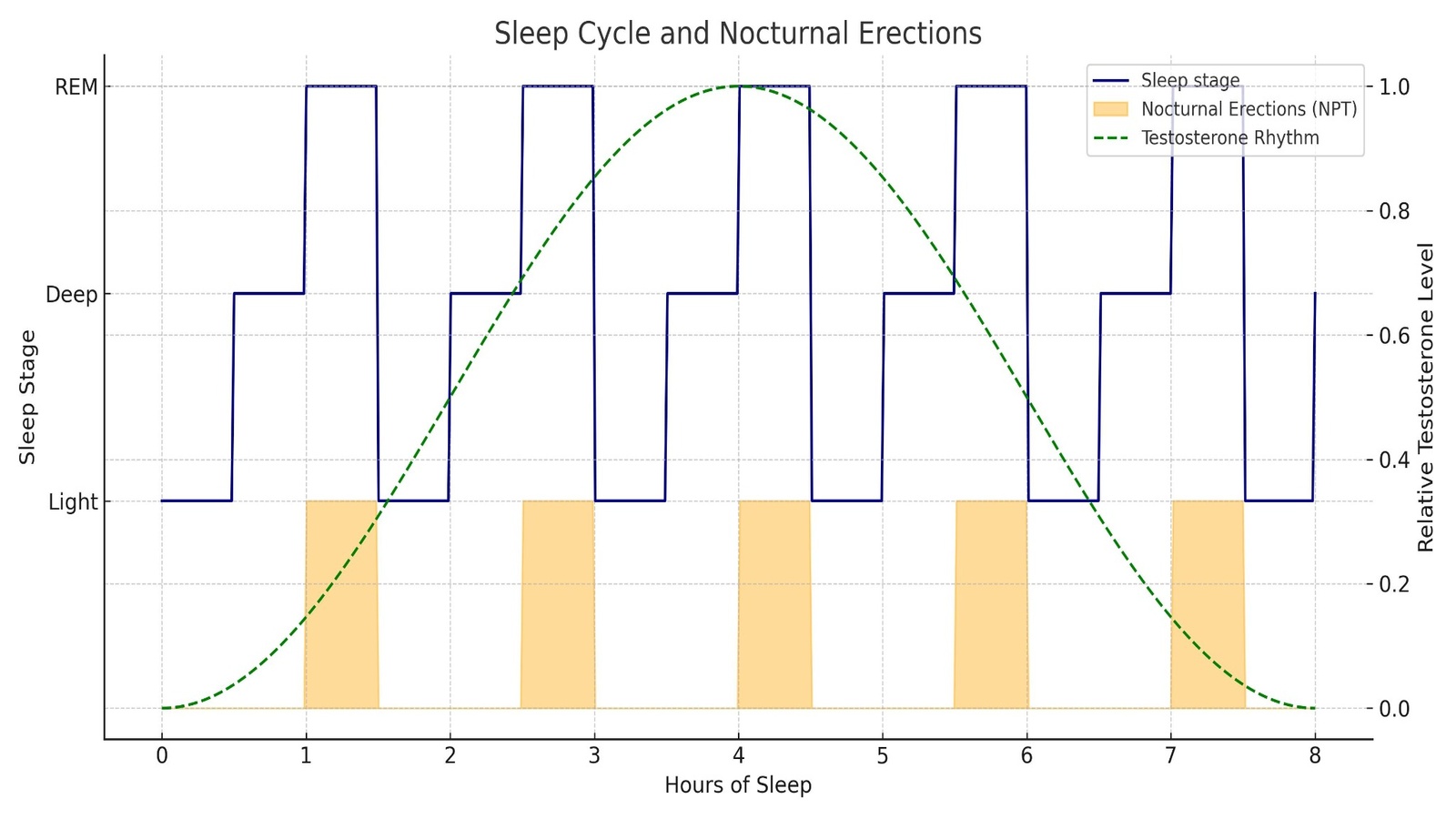
To make this easier to visualize, imagine a graph of the sleep cycle. Each time the body enters REM sleep, usually every ninety minutes, a nocturnal erection begins. Overlay that with the natural rise of testosterone toward dawn, and it becomes clear why many men wake up with a “morning erection.” An infographic showing this cycle, with REM phases aligned to testosterone peaks, illustrates how predictable and biologically necessary nocturnal erections are.
When the absence of nocturnal erections is a red flag
It is normal for nocturnal erections to fluctuate, especially if a man is stressed, tired, or has consumed alcohol. But when they are consistently absent, it often points to deeper health concerns. Cardiovascular disease is among the most common culprits, since restricted blood flow directly limits erectile capacity. Diabetes is another major factor, damaging both blood vessels and nerves. Neurological disorders such as multiple sclerosis or spinal cord injuries may also prevent these reflexes from occurring.
Hormonal imbalances, particularly low testosterone, significantly reduce the frequency and rigidity of nocturnal erections. While purely psychological erectile dysfunction usually preserves them, severe depression or long-term stress can blunt their occurrence as well. The absence of NPT may be an early signal of broader health risks that require medical attention. In fact, many urologists note that erectile dysfunction often appears years before more serious cardiovascular events, making nocturnal erections a valuable warning system.
NPT testing: the gold standard for diagnosing erectile dysfunction
Because nocturnal erections provide such critical insight, doctors rely on NPT testing when evaluating men with erectile dysfunction. In clinical settings, patients may undergo overnight monitoring in a sleep lab, or they may use portable devices such as the RigiScan at home. These devices record the frequency, duration, and rigidity of erections throughout the night.
The results are decisive. If nocturnal erections are normal but erectile issues persist during sexual activity, the cause is most likely psychological. On the other hand, if nocturnal erections are weak or absent, this suggests an organic cause such as vascular disease, diabetes, or nerve injury. This distinction allows doctors to design treatment plans that are both accurate and effective.
Comparison table: Psychogenic vs. Organic ED
| Feature | Psychogenic ED | Organic ED |
|---|---|---|
| Nocturnal erections | Present and normal | Reduced or absent |
| Onset | Sudden, situational, linked to stress | Gradual, persistent, worsens with age |
| Main triggers | Performance anxiety, depression, relationship conflict | Diabetes, hypertension, atherosclerosis, neurological injury |
| Treatment focus | Counseling, psychotherapy, stress management, PDE5 inhibitors (Viagra, Cialis) if needed | Risk-factor control, PDE5 inhibitors, hormone therapy, injections, or surgical solutions |
This table highlights why NPT remains the gold standard. A man with performance anxiety may fail during sexual encounters but still show strong nocturnal erections, whereas someone with vascular disease will lack both. Such clarity is crucial, because the treatment approach for these two groups is completely different.
How doctors use NPT results in ED treatment plans
The clinical value of nocturnal penile tumescence testing does not end with diagnosis. For urologists and andrologists, the results of NPT are a roadmap for personalized treatment. By identifying whether erectile dysfunction is psychogenic or organic, doctors can avoid unnecessary interventions and focus on the therapies most likely to succeed.
When NPT results are normal, erectile dysfunction is more likely to have psychological roots. In such cases, physicians emphasize the importance of counseling, stress reduction, and sometimes sex therapy. For many patients, short-term use of PDE5 inhibitors such as Viagra (sildenafil) or Cialis (tadalafil) helps restore confidence and break the cycle of performance anxiety.
When NPT results are abnormal, the situation points toward organic causes. Doctors then investigate cardiovascular health, blood sugar control, hormonal levels, and possible nerve injuries. Treatment plans here are more medical in nature, often requiring both lifestyle modifications and targeted therapies.
The role of PDE5 inhibitors in 2025
More than two decades after their introduction, PDE5 inhibitors remain the first-line treatment for most men with ED. They are safe, effective, and widely studied. By 2025, the four most commonly prescribed medications are:
- Sildenafil (Viagra) – still the most recognized, effective for 4–6 hours.
- Tadalafil (Cialis) – popular for its long 36-hour window of action, now available in once-daily microdoses.
- Vardenafil (Levitra) – similar to sildenafil but with a faster onset.
- Avanafil (Stendra) – the newest, offering the quickest onset (15 minutes) with fewer side effects.
These medications are not used blindly. NPT results help doctors decide whether they are appropriate. A man with intact nocturnal erections but anxiety-related ED will likely respond very well. In contrast, someone with diabetes and absent nocturnal erections may require higher doses, combination therapy, or even injectable treatments.
Beyond oral medication
When PDE5 inhibitors do not work, doctors move to second-line therapies. Alprostadil injections or intraurethral suppositories directly trigger erections by relaxing penile blood vessels. For men with severe organic ED, particularly those with absent nocturnal erections and poor vascular health, these approaches can restore function when pills fail.
Testosterone replacement therapy (TRT) also plays a role. If NPT testing shows diminished erections and bloodwork confirms low testosterone, supplementation can improve both libido and erectile function.
Case scenario 1: Psychogenic ED with normal NPT
A 38-year-old man reports difficulty maintaining erections with his partner. NPT testing shows normal erections during sleep. This points toward psychological causes. His treatment plan includes counseling, stress management, and on-demand sildenafil. Within months, his daytime erectile function improves.
Case scenario 2: Organic ED with absent NPT
A 59-year-old man with type 2 diabetes presents with progressive ED. NPT testing reveals absent nocturnal erections. This confirms organic ED. His doctor adjusts his diabetes medication, prescribes tadalafil for daily use, and later adds intracavernosal injections when pills alone prove insufficient. The NPT data helped avoid mislabeling the problem as psychological.
When to see a doctor about nocturnal erections
Occasional changes in nocturnal erections are normal. Stress, alcohol, poor sleep, or even certain medications can temporarily reduce their frequency. However, men should not ignore a consistent absence of morning or nighttime erections.
Medical evaluation is especially important if erectile dysfunction develops gradually, or if it occurs alongside other health issues such as fatigue, low libido, frequent urination, chest discomfort, or high blood pressure. These signs may point to underlying conditions like diabetes, low testosterone, or cardiovascular disease.
Modern urology emphasizes prevention. Men in their forties and fifties who notice changes in their erectile function, including a decline in nocturnal erections, should seek medical advice even if sexual activity is not a priority. Early testing often reveals risk factors that can be managed before serious complications arise.
Practical guidance for patients
If you are concerned about your nocturnal erections or erectile function in general, here are questions to consider asking your doctor:
- Could my ED be a sign of cardiovascular disease?
- Do I need an NPT test, or are other diagnostic methods enough?
- Would lifestyle changes (diet, exercise, sleep improvement) improve my erectile health?
- Which treatment option suits my condition best – oral medication, hormone therapy, or advanced interventions?
Being proactive with these questions ensures that the treatment plan is tailored to your unique health profile, rather than relying on a trial-and-error approach.
F.A.Q: Nocturnal erections and ED
Do nocturnal erections mean I am healthy?
Not always. While their presence usually indicates healthy vascular and nerve function, it does not rule out early disease. Men with heart disease or diabetes may still experience some nocturnal erections before problems worsen.
Can I have ED and still get nocturnal erections?
Yes. Men with psychogenic ED often have normal nocturnal erections. In these cases, stress, anxiety, or relationship issues may prevent erections during sexual activity, even though the physical system is intact.
What if I never notice nocturnal erections?
Many men are simply unaware of them because they occur during REM sleep. Lack of awareness does not always mean they are absent. Only an NPT test can give reliable results.
Is NPT testing available at home?
Yes. By 2025, wearable devices and portable monitors like RigiScan are widely available, making at-home NPT testing more accessible than ever.
What treatments are most effective if NPT shows organic ED?
For organic ED, first-line therapy remains PDE5 inhibitors such as Viagra (sildenafil) or Cialis (tadalafil). If these are not effective, options include hormone therapy, penile injections (e.g., alprostadil), vacuum devices, or implants.
Conclusion
Nocturnal erections are more than a biological curiosity. They are a window into men’s health, offering vital clues about vascular integrity, hormonal balance, and neurological function. By 2025, NPT testing continues to be the gold standard for distinguishing between psychogenic and organic ED.
Understanding the role of nocturnal erections empowers men to take charge of their health. Whether it means addressing psychological stress, improving lifestyle, or receiving timely medical therapy, paying attention to these nighttime events can make the difference between early prevention and late diagnosis of serious conditions.
In short, nocturnal erections are not just about sexual performance – they are about overall well-being and longevity.
References
- Cleveland Clinic Erectile Dysfunction: Causes, Diagnosis & Treatment
- Mayo Clinic Erectile dysfunction: Diagnosis & treatment
- PubMed – The Role of Nocturnal Penile Tumescence and Rigidity (NPTR) Monitoring in Differentiating Psychogenic from Organic ED
- NIH / NCBI Bookshelf – Physiology, Sleep Stages (REM sleep and penile/clitoral tumescence)
- Harvard Health Publishing – Erectile Dysfunction (ED) overview (causes & treatment options)
