Infertility affects millions of couples worldwide, and in nearly 50% of cases, male infertility is a contributing factor. With the global trend of couples starting families later in life and the rise of lifestyle-related health problems, understanding male fertility has never been more important.
In 2025, modern medicine provides patients with advanced diagnostic tools and innovative male infertility treatment options that significantly increase the chances of successful conception. This article explores the causes, diagnostic methods, treatment options, and lifestyle strategies for improving male fertility, highlighting the most effective approaches available today.
Causes and Prevalence of Male Infertility
Male infertility is defined as the inability to conceive a child despite regular, unprotected sexual intercourse for at least 12 months. According to the Mayo Clinic and the Cleveland Clinic, approximately 1 in 7 couples struggles with infertility, with male factors responsible in about 30–50% of cases.
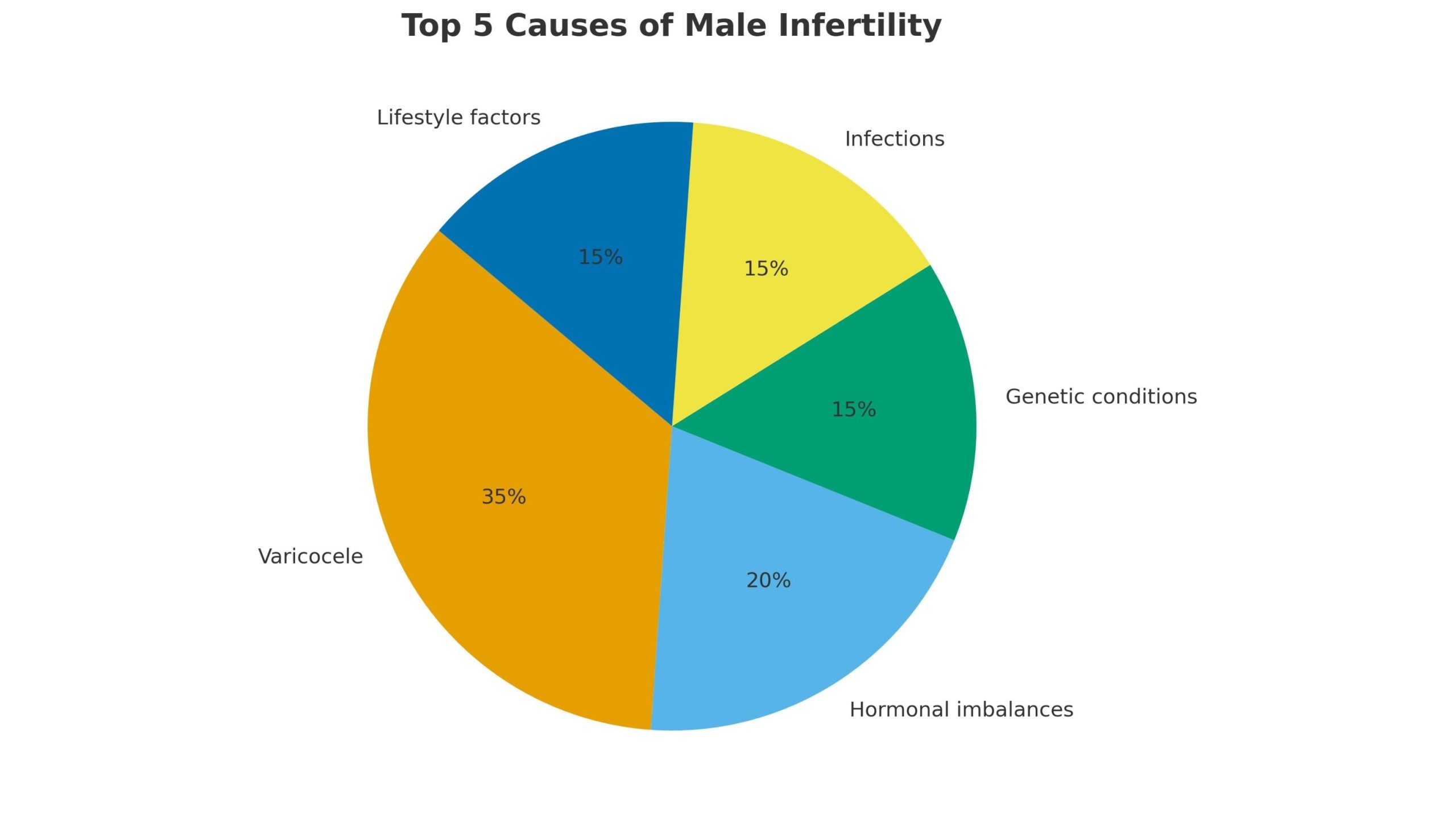
The most common causes of male infertility include:
- 1. Varicocele – enlarged veins in the scrotum that disrupt sperm production and quality.
- 2. Hormonal imbalances – low testosterone, pituitary gland disorders, or thyroid dysfunction.
- 3. Genetic conditions – such as Klinefelter syndrome or Y-chromosome microdeletions.
- 4. Infections – including sexually transmitted diseases and chronic conditions like prostatitis, which can interfere with sperm function.
- 5. Obstructions – blockages in the vas deferens or epididymis that prevent sperm transport.
- 6. Lifestyle and environmental factors – smoking, alcohol abuse, obesity, heat exposure, or toxin exposure.
Modern varicocele surgery can restore sperm parameters and improve natural conception rates
Top 5 Causes of Male Infertility.
Key point: While some causes are genetic or structural, many cases are treatable or reversible with proper male infertility treatment. For a deeper look into how medical, genetic, and environmental factors combine, see:male infertility uncovered.
Advanced Diagnostics in 2025
One of the biggest advances in male infertility treatment in 2025 is comprehensive diagnostics. Identifying the root cause is crucial, as therapy varies depending on the condition.
Modern diagnostic tools include:
- Semen analysis (computer-assisted) – Beyond sperm count and motility, new AI-driven systems evaluate sperm DNA fragmentation, morphology, and overall fertility potential.
- Hormonal testing – Measuring testosterone, FSH, LH, and prolactin levels to detect hormonal imbalances that impair sperm production.
- Genetic testing – Identifying chromosomal abnormalities or single-gene mutations associated with infertility.
- Scrotal and transrectal ultrasound imaging – Detecting varicocele, obstructions, or testicular abnormalities with greater accuracy than before.
- Advanced microbiome analysis – Research now links the gut and seminal microbiome to sperm quality and fertility outcomes.
Emerging innovation in 2025: Some urologists now use AI-powered predictive models that combine semen analysis, hormone results, and lifestyle data to suggest the most effective male infertility treatment strategy.
Medical Therapy: Antioxidants, Hormones, and Antibiotics
For many patients, the first step in male infertility treatment is medical therapy. This category includes several different approaches, but all of them are aimed at improving sperm quality and addressing underlying problems.
Antioxidants
One of the most widely discussed strategies in 2025 is antioxidant therapy. Oxidative stress remains a leading factor behind poor sperm motility and DNA fragmentation. Meta-analyses published in recent years show that antioxidants such as vitamin C, vitamin E, coenzyme Q10, and L-carnitine can modestly improve semen parameters. The effect, however, varies depending on the patient’s baseline condition and the treatment regimen, and while some couples achieve up to a 20% increase in natural conception rates, others may see no significant improvement.
Hormones
Hormonal therapy is another important option. Men with low testosterone or abnormal FSH and LH levels often benefit from treatments like clomiphene citrate, hCG injections, or aromatase inhibitors. These medications help restore the natural hormonal balance, which in turn stimulates spermatogenesis.
Antibiotics
Finally, medical therapy often includes antibiotics and anti-inflammatory agents. Infections such as prostatitis or epididymitis can seriously damage sperm function if untreated. Timely antibacterial treatment not only eliminates the infection but also prevents scarring and obstruction of the reproductive ducts.
Surgical Options: Varicocele Repair and Obstruction Removal
When structural abnormalities are the main barrier, surgical intervention becomes the cornerstone of treatment. The most common procedure is varicocele surgery, which corrects dilated scrotal veins that interfere with sperm production. Modern microsurgical and laparoscopic approaches in 2025 are minimally invasive and deliver excellent outcomes: the majority of patients experience measurable improvements in semen quality, and many couples achieve spontaneous pregnancies afterward.
Another surgical solution involves addressing blockages in the vas deferens or epididymis. Microsurgical reconstruction can restore sperm flow naturally, sometimes avoiding the need for advanced reproductive technologies altogether. For men with azoospermia, where no sperm is present in the ejaculate, procedures such as testicular sperm extraction (TESE) provide a way to retrieve viable sperm directly from the testes for use in assisted reproduction.
Assisted Reproductive Technologies (ART): IVF, ICSI, and Sperm Donation
When neither medication nor surgery is sufficient, couples often turn to assisted reproductive technologies. IVF (In Vitro Fertilization) remains the most recognized method, but in 2025 it is far more sophisticated than it was a decade ago. Success rates depend strongly on female age and clinical setting. In women under 35 in the U.S. and Europe, the average live birth rate per cycle is now around 50–55%. Some leading centers using advanced embryo selection and genetic screening report rates above 60%, but this remains the exception rather than the rule.
For severe male factor infertility, ICSI (Intracytoplasmic Sperm Injection) has become the standard of care. This technique allows embryologists to inject a single healthy sperm directly into an egg, bypassing many natural barriers. It offers a solution even in cases of extremely low sperm counts, but overall success still depends not only on the male factor but also on the quality of the eggs and, importantly, the age of the female partner.
When no viable sperm can be retrieved, sperm donation provides another pathway. Donor programs are highly regulated in the United States and other countries, ensuring both safety and genetic screening. Reported live birth rates generally range from 50% to 65% per cycle, with higher success in younger women.
Comparison of Treatment Options
| Treatment option | Typical use case | Success rate (approx.) | Invasiveness |
|---|---|---|---|
| Medical therapy | Hormonal imbalance, infections, oxidative stress | Highly variable; some couples see up to ~20% increase in natural conception | Low |
| Varicocele surgery | Correcting dilated scrotal veins | Majority show semen quality improvement; spontaneous pregnancies in many cases | Moderate |
| Obstruction removal | Blocked vas deferens or epididymis | 40–60% restoration of sperm flow | Moderate |
| TESE + ICSI | Azoospermia with sperm retrieval | Dependent on egg quality and age of female partner | High |
| IVF | General infertility, unexplained cases | ~50–55% per cycle (<35 yrs); lower with age | High |
| Sperm donation + IVF | No viable sperm available | ~50–65% per cycle, higher in younger women | High |
Lifestyle Impact on Male Fertility
Beyond medical and surgical care, everyday choices play a crucial role in male fertility. Lifestyle is one of the most modifiable factors, and positive changes often translate into better reproductive outcomes within months.
Diet plays a central role. Diets rich in fruits, vegetables, whole grains, lean proteins, and omega-3 fatty acids promote healthier sperm, while processed foods, trans fats, and excessive sugar intake are consistently linked with reduced sperm counts and motility.
Stress management is equally important. Chronic stress disrupts testosterone production and can lower sexual desire. Techniques such as mindfulness, yoga, or even structured breathing exercises are proven to restore hormonal balance and support reproductive health. A more detailed exploration of how diet, exercise, sleep, and stress interact can be found in this lifestyle-focused guide.
Sleep quality matters as well. Research up to 2025 confirms that both sleep deprivation and oversleeping are associated with lower semen quality. The ideal range is 7–8 hours per night of consistent, restorative sleep.
Finally, unhealthy behaviors such as smoking, excessive alcohol use, or frequent cannabis consumption remain major risk factors. Cutting back or quitting these habits often results in measurable improvements in semen quality within three to six months.
When to See a Urologist
According to the American Urological Association (AUA), couples should seek consultation with a urologist if they have not conceived after 12 months of regular, unprotected intercourse – or after just 6 months if the female partner is over 35.
It is also advisable to see a specialist earlier if there are:
- a history of varicocele, undescended testicles, or genital surgery,
- signs of hormonal imbalance such as fatigue, reduced libido, or erectile dysfunction,
- past infections like mumps orchitis or recurrent prostatitis,
- occupational exposure to toxins, radiation, or chemotherapy.
Early diagnosis can shorten the time to treatment and improve the chances of a successful outcome.
Frequently Asked Questions (FAQ)
How common is male infertility?
Male factors contribute to about 30–50% of infertility cases, affecting roughly 1 in 7 couples worldwide.
Can lifestyle changes alone restore fertility?
Sometimes. Improvements in diet, exercise, stress management, and sleep can boost sperm quality, especially in mild cases. But structural or genetic problems usually require medical or surgical treatment.
How effective is IVF for male infertility?
In 2025, women under 35 experience an average live birth rate of 50–55% per IVF cycle in the U.S. and Europe. Rates are lower in older age groups but can be higher in specialized centers with advanced technology.
Does varicocele always require surgery?
No. Small varicoceles without symptoms may not affect fertility. Surgery is generally recommended only when semen quality is impaired and conception has not occurred naturally.
Is male infertility permanent?
Not always. Conditions such as infections, hormonal imbalances, and varicocele can be successfully treated. Even when natural conception is not possible, advanced technologies like ICSI or donor sperm offer alternative pathways to parenthood.
Male Infertility Treatment in 2025: Key Takeaways
By 2025, men facing fertility challenges have access to more options than ever before. Modern medical therapy, minimally invasive varicocele surgery, and advanced reproductive technologies like IVF and ICSI enable physicians to design personalized treatment strategies. At the same time, lifestyle improvements and early consultation with a urologist can significantly increase success rates.
The message for couples is clear: infertility is no longer an insurmountable barrier. With evidence-based medicine, supportive lifestyle changes, and timely professional care, the dream of parenthood is within reach for most families.
